Prof. Dr. Murat Demirel, one of the best orthopedic surgeons performing shoulder muscle tear surgery in Ankara, stands out with his expertise and experience in treating damage to the shoulder joint and the muscle–tendon structures. Shoulder muscle tears usually occur due to trauma, overuse, or age-related degeneration and can seriously affect quality of life. Among the hospitals in Ankara that perform shoulder muscle tear surgery, Prof. Dr. Demirel provides care in centers equipped with advanced technology and high hygiene standards, creating surgical plans tailored to each patient’s needs.
By conducting a detailed preoperative evaluation to determine the most appropriate treatment method, Prof. Dr. Demirel closely follows his patients postoperatively as well. With medical advice after shoulder muscle tear surgery, he ensures that the recovery process progresses quickly, safely, and comfortably. In addition, by providing transparent information about shoulder muscle tear surgery prices in Ankara, he helps patients make informed decisions. You can contact us immediately to protect your shoulder health, reduce your pain, and regain your freedom of movement, and schedule an appointment.
| Disease Name | Shoulder Muscle Tear (Rotator Cuff Tear) |
| Affected Area | Supraspinatus, infraspinatus, teres minor, subscapularis muscles |
| Symptoms | Shoulder pain, limited range of motion, loss of strength, difficulty lifting the arm, night pain |
| Diagnostic Methods | Physical examination, ultrasound, MRI (to assess the location and size of the tear) |
| Causes | Repetitive microtraumas, overuse, age-related degeneration, acute trauma |
| Risk Factors | Advanced age, overhead work or sports, smoking, diabetes |
| Treatment Methods | Conservative: NSAIDs, rest, physical therapy, subacromial injection; Surgical: arthroscopic or open rotator cuff repair |
| Surgical Options | Arthroscopic rotator cuff repair, mini-open or open repair techniques |
| Complications | Re-tear, shoulder stiffness, infection, adhesions |
| Recovery Process | 4–8 weeks with conservative treatment; 4–6 months after surgery |
| Prevention Methods | Strengthening the shoulder muscles, avoiding excessive overhead strain |
| Follow-Up | Regular physical therapy check-ups, monitoring of healing with MRI |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What Is a Shoulder Muscle Tear and Why Is It So Important?
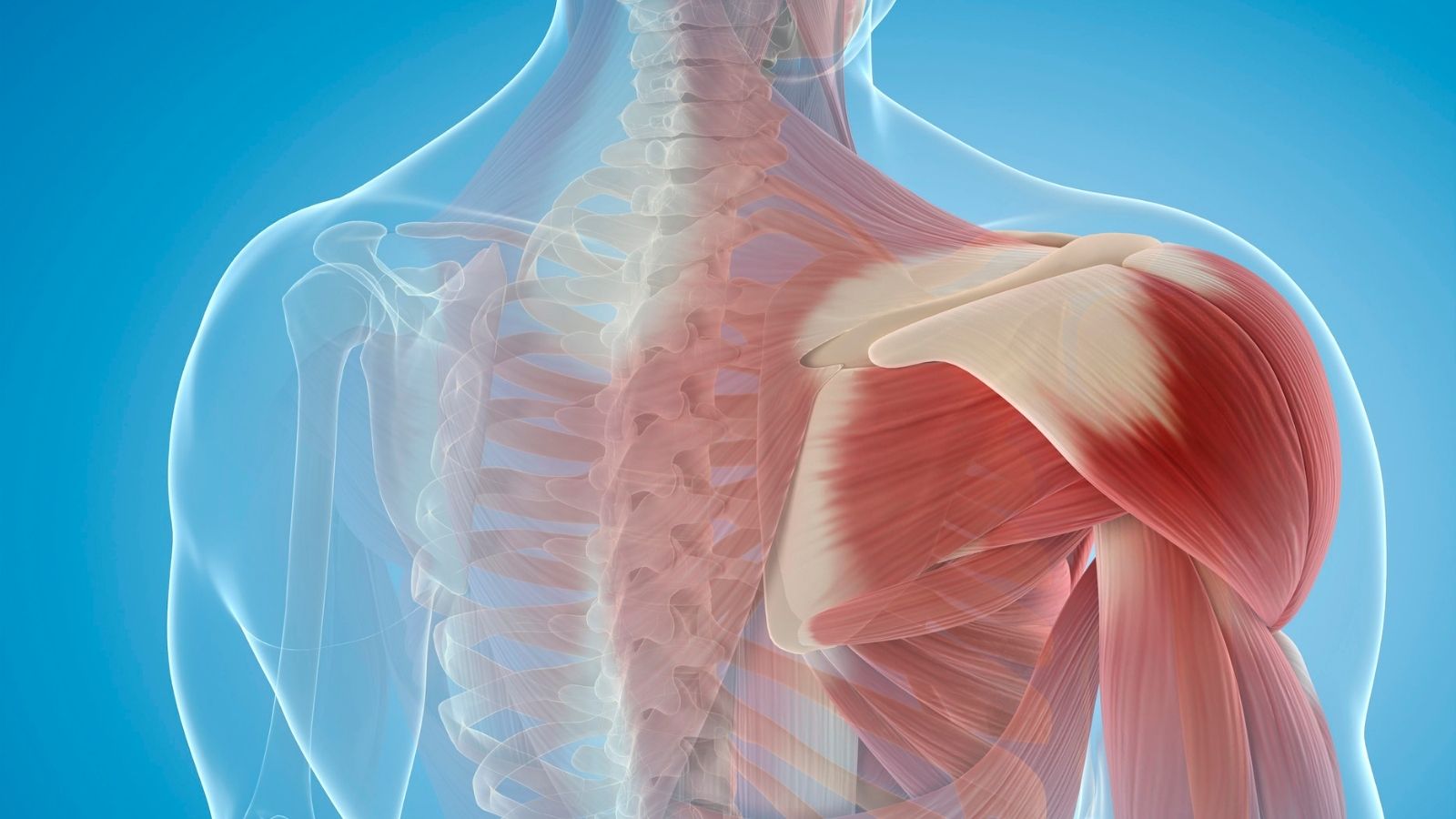
To better understand a shoulder muscle tear, let’s first look at the remarkable design of the shoulder joint. The shoulder is the most mobile joint in our body. We owe this to the round head of our upper arm bone (humerus) sitting in a shallow socket on our shoulder blade (scapula). We call this a “ball-and-socket” joint. This incredible range of motion comes at a price: by nature, it is quite an unstable structure. This can be compared to a golf ball resting on a small tee. The ball can move easily in every direction but can lose balance with the slightest jolt.
This is where the shoulder’s faithful guardians—the rotator cuff muscles—come into play. This is a combined structure formed by the tendons of four muscles. These muscles originate from the scapula and, via their tendons, attach like a cuff to the head of the humerus, keeping it centered in the socket. These four heroic muscles are:
Supraspinatus: One of the most important muscles initiating arm abduction to the side. It is generally the most stressed and most frequently torn tendon.
Infraspinatus and Teres Minor: These two muscles allow external rotation of the arm. For example, when unlocking a door with a key or performing a backhand stroke in tennis, we use these muscles.
Subscapularis: This muscle is responsible for internal rotation of the arm. It works actively when you try to move your hand behind your back to your waist.
When a shoulder muscle tear occurs, one or more of these tendons partially or completely detaches from its attachment point on the bone. If the tendon is simply worn and thinned, we call this a “partial tear.” If the tendon has completely separated from the bone, creating a gap, this is referred to as a “full-thickness tear.” This condition can lead not only to difficulty with movements like lifting or rotating the arm but also to a general loss of shoulder stability and, over time, more serious problems. Therefore, a shoulder muscle tear is an important health issue that must be taken seriously.
Why Does a Shoulder Muscle Tear Occur—Who Is the Culprit?
Shoulder muscle tears usually present in two main scenarios. Sometimes they occur due to an acute event, but more often they result from gradual wear and tear accumulated over years.
Acute Shoulder Muscle Tear
These tears are usually associated with a clear moment of trauma. For example, falling onto an outstretched arm, suddenly trying to lift a very heavy suitcase, or striking the shoulder during a traffic accident can abruptly tear even a healthy tendon. In such cases, severe pain, a sensation of “tearing,” and sudden weakness when moving the arm are typical.
Degenerative Shoulder Muscle Tear Over Time
However, the majority of shoulder tears do not result from a single event but from wear and tear caused by time and use. It is a “use and wear out” situation. Several key factors contribute to this slow-developing process.
The main factors triggering this wear-and-tear process are:
Repetitive Overhead Movements: If your job or sport constantly requires lifting your arms above your head, your rotator cuff tendons are under continuous stress. Occupations such as painters, carpenters, and electricians are at risk. Similarly, sports like swimming, volleyball, tennis, and weightlifting can cause microscopic tendon tears that eventually progress to a larger tear.
Age-Related Changes: As we age, our tendons, like all tissues, lose elasticity and resilience. More importantly, blood flow to the tendons around the shoulder decreases. Blood is the lifeline that carries oxygen and nutrients needed for tissues to repair themselves. Reduced blood flow weakens the tendon’s ability to heal small injuries, making it more prone to tearing.
Shoulder Impingement Syndrome: Sometimes, small, sharp bone spurs can form over time under the bone called the acromion, which forms the roof of the shoulder. Each time we raise our arm, the rotator cuff tendons rub against these spurs, wearing down as if against sandpaper. This constant friction first leads to tendon inflammation (tendinitis) and then sets the stage for a tear.
Often, these factors do not act alone but work together to cause the tear. For example, repetitive strenuous movements in a person in their 50s, whose tendon blood flow has already decreased, will multiply the risk of a tear.
Who Is at Higher Risk for a Shoulder Muscle Tear?
Although it can occur in anyone, certain conditions significantly increase the likelihood of developing a shoulder muscle tear. Knowing these risk factors can guide us in taking preventive measures.
We can say that the risk is higher in the following groups:
Older Adults: Age is the most important and inevitable risk factor. The risk begins to increase after the age of 40, and shoulder muscle tears are quite common in the population over 60. Sometimes they may even exist without any symptoms.
Certain Occupational Groups:
- Construction workers
- Painters
- Carpenters
- Auto mechanics
- Plumbers
Those Involved in Certain Sports:
- Tennis
- Volleyball
- Swimming
- Baseball (especially pitchers)
- Weightlifting (bodybuilding)
Those with Genetic Predisposition: Research shows that some families may have a predisposition to shoulder muscle tears. This may be related to genetic factors that determine tendon structure. In other words, if this problem is common in your family, you should be cautious as well.
Smokers: Smoking narrows blood vessels and reduces blood flow to tissues. This severely impairs tendon nutrition and self-repair capacity. Smokers not only have a higher risk of developing tears but may also experience more problematic recovery after surgery, if needed.
Those with a Unilateral Tear: A person who has a degenerative (wear-related) tear in one shoulder has a high likelihood of developing a similar problem in the other shoulder as well, because both shoulders are exposed to similar aging and wear processes.
Contact us for detailed information and an appointment!
What Symptoms Does a Shoulder Muscle Tear Cause?
The symptoms of a shoulder muscle tear can vary greatly depending on the size of the tear, how long it has been present, and the person’s activity level. However, some symptoms give a strong signal that “something is not right” in the shoulder.
The most common complaints are:
Night Pain: Perhaps the most typical and disturbing symptom. Even if pain during the day is not severe, patients often complain of pain that worsens when lying down—especially when lying on the affected shoulder—waking them from sleep.
Resting Pain: As the tear progresses, there may be a persistent aching pain even when the arm is at rest, not only with movement.
Pain with Specific Movements:
- Lifting the arm upward
- Abducting the arm to the side
- Moving the hand behind the back (such as fastening a bra or putting on a jacket)
- Reaching for an item on an overhead shelf
Weakness in the Arm: Patients often complain more about weakness than pain. Phrases like “I can’t lift my arm” or “I can’t carry the shopping bag” are common. This weakness stems from the tendon’s failure to transmit muscle force to the bone.
Sounds from the Shoulder (Crepitus): Catching, grinding, or “clicking” sounds may be heard or felt when moving the shoulder.
Limited Range of Motion: Due to pain and weakness, shoulder range of motion decreases over time. Simple daily activities like combing hair or eating can become difficult.
If the tear occurred due to an acute trauma such as a fall, symptoms also start suddenly: severe pain, a feeling of tearing in the shoulder, and inability to lift the arm at all. In degenerative tears, these symptoms appear gradually over months or even years and progressively worsen.
Which Methods Are Used to Diagnose a Shoulder Muscle Tear?
The path to proper treatment starts with an accurate diagnosis. When diagnosing a shoulder muscle tear, we piece together clues like a detective. This process consists of several important steps.
First, I listen to you carefully. When and how your symptoms began, which movements increase your pain, whether it disrupts your sleep at night, and how much it affects your daily life provide valuable information about the source of the problem. Your occupation, sports activities, and general health are also important parts of the diagnostic process.
Then I perform a comprehensive physical examination. During this exam:
Inspection: I compare both shoulders to see if there is any hollowing, swelling, or deformity.
Palpation: By gently pressing on specific points around the shoulder, I try to determine where tenderness is concentrated.
Range of Motion Assessment: I measure your active and passive range of motion by asking you to move your arm in various directions (forward, sideways, backward).
Muscle Strength Tests: I use special maneuvers designed to test the strength of each rotator cuff muscle individually. In these tests, I apply resistance in a specific direction and ask you to counter it. This provides important clues as to which tendon may be affected.
Although physical examination findings often provide a strong idea of the diagnosis, we use imaging methods to confirm it and to clearly see the location, type, and size of the tear.
X-ray: X-rays do not show soft tissues like tendons. However, they are usually the first test we request to rule out other causes of shoulder pain (such as arthritis, bone spurs, fractures) or to observe bony changes indicating that the tear has been present for a long time.
Magnetic Resonance Imaging (MRI): This is the gold standard for diagnosing shoulder muscle tears. MRI shows tendons, muscles, ligaments, and all other soft tissues of the joint in remarkable detail. An MRI report tells us:
Is there a tear or not?
Which tendon is torn?
Is the tear partial or full-thickness?
What is the size of the tear?
How far has the tendon retracted?
Is there muscle atrophy or fatty degeneration?
This information not only confirms the diagnosis but also guides us in determining the most appropriate treatment method (surgical or non-surgical).
Ultrasonography (USG): When performed by an experienced radiologist, ultrasound is a fast, lower-cost, radiation-free method that can be as effective as MRI in detecting rotator cuff tears. The ability to perform dynamic evaluation (observing tendons during movement) is an advantage.
By combining all this information (your history, my examination findings, and imaging results), we clarify the diagnosis of a shoulder muscle tear and draw up the most accurate treatment roadmap for you.
Does Every Shoulder Muscle Tear Require Surgery? What Are the Non-Surgical Options?
This is one of the most frequently asked questions by my patients, and the clear answer is “No.” Not every shoulder muscle tear—especially at the outset—requires surgery. In fact, a significant portion of patients can be relieved of pain and regain satisfactory shoulder function with well-planned non-surgical (conservative) treatments. The goal of non-surgical treatment is not to eliminate the tear (because a torn tendon generally does not heal on its own), but to control pain, reduce inflammation, and compensate for the deficient tendon by strengthening other shoulder muscles.
The main methods we use in non-surgical treatment are:
Activity Modification and Rest: This is the first and simplest step. We ask you to avoid shoulder-straining, painful movements—especially overhead activities—for a period. This allows the shoulder to rest and the inflamed tissues to settle down.
Ice Application: Applying ice to the front and side of the shoulder for 15–20 minutes, especially after activity or during painful periods, is very effective in controlling pain and swelling.
Medication: Under medical supervision, we can use nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. These medications not only relieve pain but also suppress the underlying inflammation.
Physical Therapy and Exercise: This is the backbone of non-surgical treatment. The aim is not only to reduce pain but also to restore lost range of motion and, more importantly, to strengthen the intact rotator cuff muscles and the supporting scapular muscles. Strong muscles reduce the load on the joint and help it function more stably.
Intra-articular Injections: If pain cannot be controlled by other methods and prevents the patient from participating in physical therapy, we may consider injections into the shoulder joint. Two main types are commonly used:
Corticosteroid Injection: Cortisone is a very powerful anti-inflammatory agent. When injected into the joint, it can rapidly suppress pain and inflammation, providing significant relief. However, this effect is usually temporary, and due to potential adverse effects on tendon tissue, repeated injections are avoided. Typically, it is used once or twice to create a “window of opportunity” to start physical therapy.
Biologic Treatments such as PRP (Platelet-Rich Plasma) and Stem Cells: These methods aim to trigger the body’s own healing mechanisms. They involve injecting reparative cells prepared from the patient’s own blood or obtained from bone marrow/fat tissue into the tear area. While the effectiveness of these treatments is still under investigation, they are emerging as promising options, especially for partial tears or to support healing after surgery.
Non-surgical treatment requires patience and active patient participation. Results usually begin to appear within a few weeks to a few months. If sufficient success is not achieved with these methods, surgical treatment then becomes an option.
When Is Surgical Treatment Decided for a Shoulder Muscle Tear?
Despite trying non-surgical methods, if we do not achieve the desired outcome—or in certain special cases—surgical treatment becomes the most appropriate option. The decision for surgery is not made hastily. We consider many factors when making this decision.
The main situations that lead us to consider surgery are:
Failure of Non-Surgical Treatment: Persistent pain and insufficient functional improvement despite at least 3 to 6 months of regular physical therapy, medications, and injections is the most common reason for surgery.
Size and Type of Tear: Full-thickness and large tears (usually wider than 3 cm), especially in young and active patients, are unlikely to heal on their own or recover functionally with conservative treatment. In such cases, we may recommend surgical repair before the tear enlarges and the muscles atrophy.
Acute Traumatic Tears: In a young or middle-aged active individual, a sudden full-thickness tear due to trauma (such as a fall or accident) usually requires early surgical treatment. In this situation, tendon quality is generally good, and early repair increases the chance of the best functional outcome.
Marked and Progressive Weakness: If there is severe weakness that prevents the patient from lifting the arm or performing daily tasks, this indicates a complete loss of tendon function and requires surgical repair.
Patient’s Age and Activity Expectations: In active patients who need their arms for work or sports (for example, an athlete, construction worker) and wish to return to these activities, surgery may be prioritized to restore function to the highest level.
The decision for surgery is a shared one, made after discussing your expectations, lifestyle, and the characteristics of your tear in detail. Every patient and every tear is different; therefore, the treatment plan must be personalized.
How Is Shoulder Muscle Tear Surgery Performed?
The main goal of shoulder muscle tear surgery is to reattach the torn tendon, which has separated from the bone, back to its original footprint on the head of the humerus. Thanks to modern technology, we can perform this repair effectively and comfortably for the patient.
The principal surgical techniques we use are:
Arthroscopic Repair (Minimally Invasive): Today, this is considered the “gold standard” for rotator cuff repair. Through several small (about half-centimeter) incisions around the shoulder, a thin instrument with a camera (arthroscope) and specially designed miniature surgical tools are introduced into the joint. The camera allows us to view all joint structures in detail on a screen. Then, we repair the torn tendon by placing small screws with very strong sutures, called “anchors,” into the bone. We pass these sutures through the tendon and tie them using special knot techniques, firmly fixing the tendon to the bone. The biggest advantages of this method are:
- Less tissue damage
- Less postoperative pain
- Smaller scars and better cosmetic results
- Faster recovery and earlier start to rehabilitation
- Lower risk of infection
Open Repair: This traditional method requires a larger surgical incision over the shoulder. Today, due to the success of arthroscopic techniques, it is preferred for very large, complex, difficult-to-repair tears or special situations requiring additional procedures (such as tendon transfers).
Mini-Open Repair: This technique combines minimally invasive and open approaches. A smaller incision is used, and the repair is performed under direct visualization.
During surgery, we not only repair the tear. If there is a bone spur causing impingement, we also shave it (acromioplasty) in the same session to create space for the tendon to move comfortably. If there are other accompanying problems (such as biceps tendon pathology), we address them as well. The success of the surgery depends not only on repairing the tear but also on properly managing such accompanying issues.
What Awaits Me After Shoulder Muscle Tear Surgery?
Surgery is only half of the equation. The other—and perhaps more important—half is the postoperative recovery and rehabilitation process. The biological process of the repaired tendon reattaching to the bone takes time. Being patient and strictly following your doctor’s and physiotherapist’s instructions is vital for a successful outcome.
The recovery process generally progresses through specific stages:
Stage One: Protection Phase (Usually the first 4–6 weeks):
- After surgery, your arm will be in a special sling to protect the shoulder.
- It is very important to wear this sling continuously except for the exercises shown to you and during bathing.
During this period, you must not lift, push, or pull anything with your operated arm. The goal is to avoid placing any load on the repaired tendon.
Your physiotherapist will perform only passive movements (not using your own muscle power) to prevent joint stiffness.
Stage Two: Regaining Mobility (Usually from week 6 to week 12):
- During this period, the sling is gradually discontinued.
- You begin exercises aimed at moving your arm using your own muscle power without assistance (active movements).
- The goal is to restore normal shoulder range of motion without pain.
- Stage Three: Strengthening Phase (Usually from month 3 to month 6):
- Once we are confident that the repaired tendon has healed sufficiently, we begin true strengthening exercises.
- In this phase, resistance bands and light weights are used to strengthen the rotator cuff muscles and the surrounding shoulder muscles.
- This is the most critical phase to increase shoulder stability and endurance.
Stage Four: Return to Activity (Usually after month 6):
- At this stage, a gradual return to sports or strenuous physical activities is targeted.
- Sport-specific movements and more advanced strengthening exercises are performed.
Remember, full recovery and regaining former shoulder strength can take 9 months to 1 year. During this period, your greatest ally will be a specialized physiotherapist. Full adherence to the rehabilitation program is the most important factor that directly affects the success of the surgery.
Contact us for detailed information and an appointment!
Frequently Asked Questions
Can a shoulder tear heal without surgery?
Not all tears are the same. The size and type of the tear (partial or full-thickness), your age, and your expectations determine the treatment. Especially small and partial tears can improve without surgery with proper physical therapy and medications, allowing you to live pain-free. However, full-thickness and large tears generally do not heal on their own; surgery may be necessary in such cases.
Is heat or cold better for a shoulder muscle tear?
Initial treatment should always be cold. Applying ice to your shoulder within the first 48–72 hours after the tear reduces bleeding and swelling, helping to control pain. After this acute phase subsides—once the swelling goes down—heat can be used to increase blood flow and relax muscles. Especially using heat before exercise and cold afterward is a good approach.
Will a shoulder muscle tear show up on MRI?
Yes, absolutely. MRI (Magnetic Resonance Imaging) is the imaging method that shows soft tissues such as muscles and tendons in the shoulder in the greatest detail. MRI clearly reveals the location, size, and degree of degeneration of the tear, confirming the diagnosis and allowing us to plan the most appropriate treatment.
Is a shoulder tear dangerous?
It is not life-threatening, but it can significantly reduce your quality of life. An untreated tear may enlarge over time, leading to severe pain, inability to lift the arm, weakness, and restricted motion. In the long term, it may cause shoulder osteoarthritis, resulting in permanent deterioration of shoulder function.
How should people with shoulder pain sleep?
Do not sleep on your painful shoulder. The ideal position is on your back. If you sleep on your side, lie on the non-painful side and support your painful arm with a pillow underneath. This reduces pressure on the joint and helps relieve night pain. Some patients are more comfortable in a semi-upright position (for example, in a recliner).
When is shoulder pain dangerous?
Pain that wakes you at night and does not improve with rest is important. If pain is accompanied by high fever, swelling, and redness in the shoulder; if severe pain starts suddenly after trauma such as a fall; or if you cannot lift your arm at all, you should see a doctor without delay. These may be signs of conditions requiring urgent intervention.
How many months does it take for a shoulder tear to heal?
The recovery time depends entirely on the type and size of the tear and the treatment method. With non-surgical treatments, improvement in pain and function may take several weeks to a few months. After surgery, recovery is longer; with physical therapy, full functional recovery typically takes 4 to 6 months and can sometimes extend to a year.
Which department treats shoulder muscle tears?
The Orthopedics and Traumatology department is responsible for diagnosing and treating disorders of the shoulder muscles, tendons, and joint. You should consult an Orthopedics and Traumatology specialist for your complaints.
Is surgery mandatory for a shoulder tear?
No, surgery is not mandatory for every shoulder tear. The decision depends on the tear size, the patient’s age, occupation, activity level, and pain severity. Surgery is a strong option for patients who do not improve with physical therapy, injections, and medications or who cannot use their arm functionally.
Which doctor should I see for shoulder pain?
The primary specialty to consult for shoulder pain is Orthopedics and Traumatology. After examination and tests, the orthopedic specialist will establish the correct diagnosis and initiate the most suitable treatment for you.
Is PRP used for shoulder muscle tears?
Yes, PRP (Platelet-Rich Plasma) therapy is one of the modern methods we use in shoulder muscle tears, especially partial tears. By injecting this fluid—rich in reparative cells and prepared from your own blood—into the tear area, we aim to enhance the body’s self-repair potential. Although not suitable for every patient, it is an effective treatment option in selected cases.