Prof. Dr. Murat Demirel, one of the best orthopedic doctors performing shoulder dislocation surgery in Ankara, is a reliable name with many years of experience in the treatment of recurrent shoulder dislocations and shoulder joint instability. Shoulder dislocations usually occur as a result of sports injuries, falls, or trauma, and if not treated correctly and on time, they can cause permanent damage to the joint. Prof. Dr. Demirel, among the hospitals performing shoulder dislocation surgery in Ankara, provides services in centers equipped with modern surgical techniques and advanced medical equipment, applying personalized surgical plans for each patient.
Prof. Dr. Demirel makes an accurate diagnosis through detailed examinations and imaging methods before surgery, and closely monitors his patients after the operation. With post-surgery doctor recommendations, he ensures that the recovery process progresses quickly, safely, and comfortably. In addition, he provides transparent and up-to-date information about shoulder dislocation surgery prices in Ankara, helping his patients make informed decisions. You can also protect your shoulder health, improve your mobility, and prevent recurrent dislocations by contacting now and making an appointment.
| Disease Name | Shoulder Dislocation (Glenohumeral Dislocation) |
| Affected Area | Shoulder joint (humeral head and glenoid cavity) |
| Symptoms | Sudden and severe shoulder pain, deformity, limited movement, swelling, and tenderness in the shoulder |
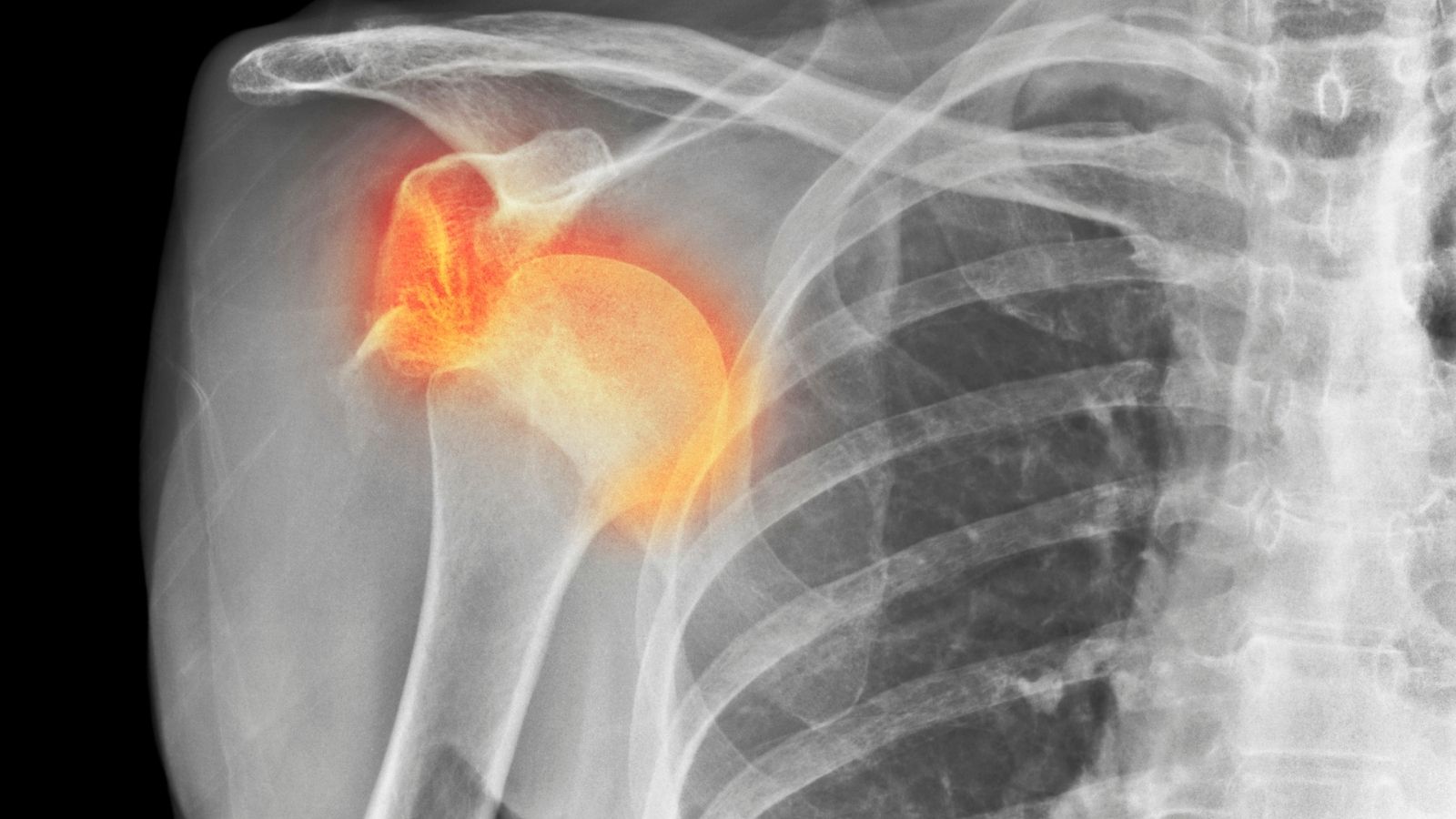
| Diagnostic Methods | Clinical examination, X-ray (to see the direction of the dislocation and accompanying fractures), MRI (to evaluate the labrum, ligaments, and muscle structures) |
| Causes | Trauma (fall, impact), sudden strain, recurrent instability conditions |
| Risk Factors | Young age, sports activities (especially contact sports), ligament laxity, previous history of dislocation |
| Treatment Methods | Closed reduction (in emergency), rest, arm sling, physical therapy; surgical stabilization in frequently recurring cases |
| Surgical Options | Arthroscopic Bankart repair, open stabilization surgeries |
| Complications | Recurrent dislocation, Bankart lesion, Hill-Sachs lesion, nerve injury (especially axillary nerve) |
| Recovery Process | 4–6 weeks with conservative treatment after the first dislocation; 3–6 months after surgery |
| Prevention Methods | Strengthening shoulder muscles, protective measures in contact sports |
| Follow-up Process | Clinical examination, MRI, and/or evaluation of physical therapy progress |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What are the common causes of shoulder dislocations?
The underlying story behind a shoulder dislocation is different for every patient. Sometimes it starts with a sudden and severe event, while other times it is the result of a slow-developing process. Understanding how shoulder dislocations occur is the first step for both treatment and prevention.
Traumatic Shoulder Dislocations: The Most Common Scenario
This is the classic and most common cause of shoulder dislocations. It usually occurs when an unexpected, sudden, and severe force pushes the shoulder beyond its normal range of motion. These scenarios may sound familiar to you.
Falls: Falling uncontrollably on an outstretched hand or arm is one of the most common mechanisms of shoulder dislocations. The entire body weight forces the shoulder, pushing the head of the arm bone out of its socket.
Sports Injuries: Colliding with an opponent in football, a wrong move in wrestling, battling for a rebound in basketball, or over-stretching the shoulder while spiking in volleyball often cause shoulder dislocations, especially in young and active individuals.
Traffic Accidents: Hitting the steering wheel or dashboard during an accident, or the seatbelt suddenly pulling on the shoulder, can also lead to severe shoulder dislocations.
In these traumatic events, the shoulder is usually forced into an open and upward position, and the head of the arm bone moves forward, creating the “anterior dislocation” type, which accounts for more than 95% of all shoulder dislocations.
Atraumatic Shoulder Dislocations: Instability Without Trauma
In some cases, the shoulder can dislocate without a significant accident or injury. This usually stems from the individual’s structural characteristics.
General Ligament Laxity (Hyperlaxity): Some people genetically have looser and more flexible connective tissue than normal. Commonly described as “loose joints,” this condition makes the shoulder joint less stable by birth and can lead to dislocation even with minimal strain, sometimes even while turning in sleep. This condition usually affects both shoulders, and the instability can be multidirectional (forward, backward, and downward).
Repetitive Microtraumas: In people who frequently perform overhead activities, such as swimmers, volleyball players, tennis players, or ceiling painters, shoulder ligaments gradually stretch and loosen over time. Even without a single major trauma, the accumulation of thousands of repetitive strains weakens the joint capsule and paves the way for instability.
Less Common Causes of Shoulder Dislocations
Posterior shoulder dislocations are much rarer and are usually associated with special circumstances. These occur when the arm bone head is pushed backward due to sudden and very strong muscle contractions.
Epileptic seizures
Electric shock
Since these situations may be overlooked during diagnosis, listening carefully to the patient’s history is critically important.
What are the symptoms of a shoulder dislocation and what should be done in such a case?
A shoulder dislocation usually presents with clear and uncomfortable symptoms that cannot be ignored. Recognizing these symptoms is important to understand the seriousness of the condition and to answer the question “how to recognize a dislocated shoulder?”. The main findings when a shoulder dislocation occurs are as follows.
Sudden and Severe Pain: Usually described as a sharp, stabbing pain at the moment of injury. The pain is so intense that the person cannot even think of moving the arm.
Visible Deformity: This is the most typical symptom. Compared to the healthy shoulder, the dislocated shoulder loses its normal rounded shape and appears more angular or “drooping.” Especially in anterior dislocations, an abnormal bony protrusion can be felt or seen at the front of the shoulder.
Complete Loss of Movement: The person cannot move the arm in any direction. The arm is usually held close to the body in a helpless position, supported by the other hand.
Muscle Spasms: The body involuntarily contracts the shoulder muscles to protect the injured area. These spasms may worsen the pain and make it harder to reposition the dislocation.
Swelling and Bruising: Within hours after the injury, swelling and bruising due to bleeding develop in the shoulder area.
Numbness and Tingling: Sometimes numbness, tingling, or a “pins and needles” sensation radiates to the arm, hand, or fingers. This indicates that important nerves around the shoulder are stretched or compressed during the dislocation and requires urgent evaluation.
What are the symptoms of a partial shoulder dislocation?
Sometimes the shoulder does not fully dislocate but only temporarily slips out of the socket and returns. This is called “subluxation” or partial dislocation. Symptoms may be milder:
- A sudden sensation of “slipping out” or “giving way” in the shoulder
- Sharp but short-term pain
- A brief feeling of weakness or “dead arm” afterward
If you experience any of these symptoms, especially if there is a visible deformity, the only thing you should do is immediately go to the nearest emergency room. Trying to reposition the shoulder by yourself or with the help of others can cause irreversible damage to the ligaments, cartilage, nerves, and even blood vessels. This is an emergency requiring professional medical care.
Contact us for detailed information and an appointment!
How is the diagnosis of shoulder dislocations made by a specialist doctor?
The diagnosis of shoulder dislocation usually begins when the patient presents to the emergency room and progresses through careful steps. This process not only confirms the presence of the dislocation but also identifies any accompanying injuries to create the most accurate treatment plan.
Listening to You: Medical History
First of all, your story is listened to.
How did the injury happen? (Did you fall, did you take a blow?)
When and how did the symptoms start?
Is this your first shoulder dislocation? Have you experienced a similar problem before?
Have you always felt looseness or insecurity in your shoulder?
Have you experienced any special situations such as seizures or electric shock?
The answers to these questions provide valuable clues about the type of dislocation and underlying causes (traumatic, atraumatic, etc.).
Careful Examination: Physical Assessment
Next, a comprehensive physical examination of your shoulder is performed. Both shoulders are compared during this examination.
Inspection: The shoulder is checked for deformity, swelling, bruising, or asymmetry. Typical signs such as the “epaulet sign” (loss of shoulder roundness and angular appearance) in anterior dislocations are looked for.
Palpation: Bone structures and soft tissues around the shoulder are examined by hand to detect tenderness, spasm, or abnormal bony protrusions.
Neurovascular Examination: One of the most critical steps. Arm pulses are checked. Sensory loss or numbness in the fingers and arm is evaluated. Strength of specific muscles (such as the deltoid innervated by the axillary nerve) is tested to assess for nerve injury. This exam must be performed both before and after reduction.
Stability Tests: These tests are usually not performed in acute dislocation due to pain. However, in patients with recurrent dislocations, special tests such as the “apprehension test” or “sulcus sign” may be applied to assess the direction and degree of looseness.
Looking Inside: Imaging Methods
Imaging methods are used to confirm physical examination findings and clarify the intra-articular condition.
X-ray: The gold standard for suspected shoulder dislocation. An X-ray clearly shows where the humeral head is relative to the socket, confirming the presence and direction of the dislocation (anterior, posterior, inferior). It also detects accompanying fractures (such as at the socket rim or humeral head).
Computed Tomography (CT): Used for detailed examination of bone structures. It is very valuable for measuring bone loss in the glenoid or humeral head after recurrent dislocations. This information is critical in deciding on surgical procedures (such as the need for a Latarjet operation).
Magnetic Resonance Imaging (MRI): MRI is the king for evaluating the shoulder’s soft tissues (ligaments, labrum, capsule, rotator cuff tendons). Especially in surgical candidates, it helps visualize Bankart lesions, ligament injuries, cartilage damage, or rotator cuff tears in detail.
This three-step evaluation process provides a personalized and most effective treatment roadmap for each patient.
What are the different types and classifications of shoulder dislocations?
Although shoulder dislocation may seem like a single condition, it is actually an injury that can occur in different directions and for different underlying reasons. Correct classification of these types is very important to determine the most appropriate treatment strategy.
Types by Direction of Dislocation
This is the most basic classification and indicates the direction in which the humeral head shifts relative to the socket.
Anterior Dislocation: By far the most common type of shoulder dislocation, accounting for more than 95% of cases. The humeral head shifts forward out of the socket.
Posterior Dislocation: Much rarer. The humeral head shifts backward behind the socket. It often has a higher risk of being overlooked.
Inferior Dislocation (Luxatio Erecta): The rarest and most dramatic type. The humeral head shifts downward, and the patient holds the arm fixed above the head.
Classification by Story: TUBS and AMBRI
To better understand shoulder instability (the tendency of the shoulder to repeatedly dislocate or feel loose), a classification based on the underlying “story” is used. It defines two main groups.
TUBS Type Instability: Usually the result of a single major event.
Traumatic: Begins after a clear injury such as a fall or accident.
Unilateral: Usually affects only one shoulder.
Bankart Lesion: Almost always accompanied by a tear of the labrum (Bankart lesion).
Surgery: These instabilities usually require surgical treatment to repair the underlying anatomical damage.
AMBRI Type Instability: Usually due to structural features of the individual.
Atraumatic: Occurs spontaneously or with very mild strain without significant trauma.
Multidirectional: The shoulder is usually loose in more than one direction (forward, backward, and downward).
Bilateral: Often both shoulders are affected, suggesting general ligament laxity.
Rehabilitation: These instabilities usually respond well to physical therapy and rehabilitation programs focused on strengthening muscles and improving shoulder control.
Inferior Capsular Shift: If surgery is needed, a special technique is used to tighten the loose joint capsule.
What are the non-surgical treatment options for shoulder dislocations and who are they suitable for?
After successful closed reduction of a shoulder dislocation, the treatment process enters a new phase. Not every shoulder dislocation requires surgery. Non-surgical (conservative) treatment methods can be successfully applied, especially in patients who have experienced their first dislocation, are older, or do not engage in high-risk sports. The philosophy of non-surgical treatment is to give the body time and support for its natural healing potential while safely restoring shoulder function.
This treatment approach consists of several key components.
Immobilization (Rest with Sling)
After reduction, your arm will remain in a sling for a period of time, usually between 2 to 4 weeks.
The aim is to allow the stretched or torn joint capsule and ligaments time to start healing. Keeping the shoulder immobile prevents further strain on these delicate tissues.
Important Note: Even while in the sling, it is important to perform hand, wrist, and elbow movements within your doctor’s or physiotherapist’s permission to prevent stiffness in these joints.
Medication and Cold Therapy
In the early days of recovery, it is important to control pain and swelling.
Cold Therapy: Applying ice packs regularly (every 2-3 hours for 15-20 minutes) to the shoulder during the first 48-72 hours helps reduce swelling and pain.
Medication: Your doctor may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) or simple painkillers to reduce pain and inflammation.
Physical Therapy and Rehabilitation: The Cornerstone of Treatment
The success of non-surgical treatment largely depends on a well-planned physical therapy program and the patient’s full compliance. This is not a passive process but a journey requiring your active participation. The program is usually phased.
Phase 1: Range of Motion: After the sling is removed, the first goal is to prevent stiffness (frozen shoulder). Gentle passive and assisted range of motion exercises are started under physiotherapist supervision. Pendulum exercises are a classic beginning.
Phase 2: Strengthening: As range of motion increases and pain decreases, focus shifts to strengthening the dynamic stabilizers of the shoulder, especially the rotator cuff and scapular muscles. Exercises progress from no resistance to elastic bands and light weights.
Phase 3: Function and Control: When shoulder strength reaches a certain level, work on neuromuscular control and proprioception begins. This improves preparedness and control against sudden movements, reducing the risk of recurrence.
Non-surgical treatment is generally the first choice for patients with a first-time dislocation, over 40 years old, with a sedentary lifestyle, or instability due to general ligament laxity (AMBRI type). However, every patient is different, and treatment decisions should be individualized.
When should surgical treatment, that is, shoulder dislocation surgery, be considered?
Although non-surgical treatment is effective for many patients, in some cases it may not provide a permanent solution and cannot prevent recurrent shoulder dislocations. At this point, surgical treatment, meaning shoulder dislocation surgery, comes into consideration to permanently restore shoulder stability and improve the patient’s quality of life. The surgical decision depends not only on the number of dislocations but also on the patient’s age, activity level, expectations, and most importantly, the severity of anatomical damage to the shoulder.
The main situations where surgical treatment is strongly considered are as follows.
Recurrent Shoulder Dislocations (Chronic Instability): If the shoulder continues to dislocate frequently or if there is a persistent sense of instability despite proper rehabilitation, this indicates unresolved structural issues. This is the most common reason for surgery.
Young and Active Patients: In patients under 25 years old who are active and athletic, the recurrence risk after the first dislocation can be as high as 80–90%. Since each new dislocation causes further damage to cartilage and bone, surgical treatment may be recommended even after the first dislocation to prevent long-term harm.
High-Risk Sports and Professions: Athletes engaged in contact or overhead sports such as football, wrestling, basketball, or volleyball usually require surgical stabilization to return to their activities safely. Similarly, individuals in physically demanding professions may benefit from surgery as a more permanent solution.
Significant Structural Damage: Imaging methods (MRI or CT) may reveal severe injuries that can only be corrected with surgery.
Torn and detached Bankart lesion
Bony Bankart lesion causing significant glenoid bone loss
Large Hill-Sachs lesion in the humeral head leading to instability
Large rotator cuff tear accompanying the dislocation
Failure of Non-Surgical Treatment: If the patient still experiences pain, loss of function, and instability despite completing a well-managed non-surgical treatment and rehabilitation program, surgery becomes the next logical step.
Irreducible Dislocation: Rarely, a piece of soft tissue may block the reduction, making it impossible to reposition the shoulder with closed maneuvers. In this case, urgent surgery is required.
The surgical decision is a personalized one made jointly by the orthopedic and traumatology specialist and the patient, weighing all these factors. The goal is not only to stop the dislocations but also to protect the long-term health of the shoulder joint and minimize the risk of arthritis in the future.
What are the current surgical methods applied in the treatment of shoulder dislocations?
Surgical treatment for shoulder instability has been revolutionized in recent years with the development of arthroscopic, minimally invasive techniques. Today, most shoulder dislocation surgeries are performed through a few small incisions using a camera and special instruments, instead of large open incisions. The choice of surgical technique depends on the patient’s individual condition and the specific intra-articular damage. The two most commonly used modern approaches are as follows.
Arthroscopic Bankart Repair: Repairing the Tear
This is one of the “gold standard” methods for treating traumatic shoulder instability and is ideal for patients without significant glenoid bone loss.
The goal of this surgery is to reattach the labrum (Bankart lesion) and the loosened capsule-ligament complex that were torn away during dislocation back to their original anatomical position.
The surgeon visualizes the inside of the joint with an arthroscopic camera. Then, small anchors with sutures (suture anchors) are placed into the glenoid bone. The sutures are passed through the torn labrum and tied to the anchors, securely fixing the labrum back to the bone. This restores the natural “bumper” in front of the shoulder and stabilizes the joint.
Advantages: Being minimally invasive, this method offers less pain, faster recovery, and better cosmetic results.
Latarjet Procedure: Reinforcement with Bone Support
This is a highly effective reconstructive surgery reserved for more complex and severe shoulder instability cases. It is especially preferred in the following situations.
- When there is significant bone loss in the anterior glenoid rim (usually more than 20–25%).
- After recurrent failed Bankart repair surgeries.
- In athletes engaged in very high-risk contact sports such as wrestling.
This surgery not only repairs soft tissues but also restores the missing bone in the anterior glenoid.
In this procedure, a small piece of bone is taken from another part of the scapula (the coracoid process) along with the attached tendons. This bone block is transferred and fixed with screws to the deficient area of the glenoid rim.
The Triple Effect: The success of the Latarjet procedure comes from its triple stabilizing effect.
- Bone Block Effect: The transferred bone increases the socket’s surface area, physically preventing the humeral head from slipping forward.
- Sling Effect: The transferred tendons act like a sling beneath the humeral head when the arm is in risky positions, providing dynamic stability.
- Capsule Repair: The shoulder capsule is repaired over the bone graft, adding further static stability.
Remplissage Procedure: Filling the Defect
This is often performed in addition to Arthroscopic Bankart repair. If the patient has a large Hill-Sachs lesion contributing to instability, the posterior capsule and rotator cuff tendons are sutured into the defect, preventing engagement with the glenoid rim.
Applying the correct technique to the right patient is crucial for a successful surgical outcome. An experienced orthopedic surgeon will evaluate all individual factors to create the most suitable surgical plan.
How does the recovery and rehabilitation process progress after shoulder dislocation treatment?
The success of shoulder dislocation treatment is not limited to the medical intervention or surgery itself. The true journey begins afterward, with recovery and rehabilitation that require patience, determination, and active participation from the patient. This process aims to restore the shoulder’s strength, mobility, and most importantly, stability. Recovery time may range from several months to a year depending on the treatment method (surgical or non-surgical) and individual factors.
General Rehabilitation Phases
The rehabilitation program is usually divided into phases based on time frames and functional goals.
Phase 1: Protection and Early Motion (First 0–6 Weeks)
- The motto of this phase is “protect and calm.”
- Goal: Protect healing tissues, control pain and swelling, and prevent stiffness (frozen shoulder).
- Applications:
- The arm is kept in a special sling for 4–6 weeks.
- Regular ice applications are performed on the shoulder.
- The shoulder is not actively used during this period.
- Gentle passive range of motion and pendulum exercises are performed under physiotherapist guidance.
- Elbow, hand, and wrist movements are actively performed.
Phase 2: Restoring Range of Motion and Light Strengthening (6–12 Weeks)
- During this phase, the shoulder is gradually “awakened.”
- Goal: Restore full, pain-free range of motion and start light activation of stabilizing muscles.
- Applications:
- Sling use is usually discontinued at the beginning of this phase.
- Active-assisted and later active range of motion exercises are started.
- Isometric and light resistance strengthening exercises (using elastic bands) for the rotator cuff and scapular muscles are introduced.
Phase 3: Strength, Endurance, and Control (3–5 Months)
- Now it’s time to rebuild the shoulder.
- Goal: Increase shoulder strength, endurance, dynamic stability, and neuromuscular control.
- Applications:
- Progressively increase resistance and weight in exercises.
- Add more functional exercises involving the kinetic chain (legs, core, and arms).
- Incorporate closed- and open-chain exercises for better adaptation to different loading types.
Phase 4: Advanced Strengthening and Return to Sport (5–6 Months and Beyond)
- This is the final and most challenging stage for athletes and physically active individuals.
- Goal: Prepare the patient safely for sport- or activity-specific movements.
- Applications:
- Plyometric exercises (e.g., medicine ball throws).
- Agility and reaction drills.
- Sport-specific drills (throwing, pushing, pulling motions).
- Gradual return to controlled contact in contact sports.
The decision to return to sports or heavy activity is not based solely on time. It is made when objective criteria such as full range of motion, absence of pain, adequate muscle strength (usually 90% compared to the healthy side), and successful functional test results are met, with the approval of the doctor and physiotherapist.
Contact us for detailed information and an appointment!
Frequently Asked Questions
How many days does it take for a shoulder dislocation to heal?
The healing time of a shoulder dislocation varies depending on the individual and the type of treatment. After the shoulder joint is repositioned, it usually requires wearing a sling for about 3–4 weeks. With physical therapy that follows, regaining the shoulder’s strength and mobility can take between 6 to 12 weeks. Especially for athletes, returning to the field may take longer. Patience and following your doctor’s recommendations are the most important factors.
How can you tell if the shoulder is dislocated?
It is usually not difficult to recognize a shoulder dislocation. First of all, there is severe pain. There will be a visible deformity in the shoulder, as if there is a gap or abnormal protrusion. Moving the arm becomes extremely difficult, sometimes impossible. Most of the time, you feel the need to support your injured arm with your healthy hand. Swelling and bruising in the front of the shoulder are also common symptoms.
Is shoulder dislocation very painful?
Yes, shoulder dislocation is a very painful condition. In fact, it is considered one of the most painful conditions in traumatology. The pain is caused by damage to tissues, nerves, and muscles when the bone comes out of its socket. The pain is so intense that patients usually rush to the emergency room. The pain continues until the shoulder is repositioned and may still be felt as tenderness for a while afterward.
Can a shoulder dislocation heal without surgery?
Yes, most shoulder dislocations, especially the first-time cases, can be treated without surgery. The treatment begins with “reduction,” which means repositioning the shoulder under anesthesia or strong painkillers. Afterward, with the use of a sling and physical therapy, the ligaments and muscles around the joint are given time to heal and strengthen. However, if dislocations recur frequently or if there is significant joint damage, surgical treatment may become necessary.
Can you move your arm when the shoulder is dislocated?
At the moment of dislocation, moving the arm is nearly impossible and extremely painful. Since the joint is not in its normal position, the muscles and nerves cannot function properly. The patient usually holds the arm close to the body, immobilized. Even after the shoulder is repositioned, movement restrictions may continue for a while, but these improve over time with physical therapy.
Is ice good for a shoulder dislocation?
Absolutely yes! Applying ice is one of the first things to do when a shoulder dislocation occurs. Ice constricts blood vessels, reducing internal bleeding and swelling (edema). It also acts as a natural pain reliever to provide some relief. The best way is to wrap the ice in a towel and apply it for 15–20 minutes at intervals. This helps control pain and damage until you reach a doctor.
Does a shoulder dislocation heal on its own?
A shoulder dislocation is not a “self-healing” condition. Rarely, the shoulder may slip back into place on its own, but this does not repair the underlying damage. A shoulder must always be repositioned properly (reduced) by a specialist doctor, followed by appropriate treatment planning. Otherwise, permanent joint damage, recurrent dislocations, and arthritis may occur.
Can a shoulder dislocation be seen on X-ray?
Yes, X-ray is the gold standard in diagnosing a shoulder dislocation. The X-ray clearly shows the position of the bones in the shoulder joint and confirms whether there is a dislocation. It also helps detect any accompanying fractures. Sometimes MRI (Magnetic Resonance Imaging) may also be requested to evaluate ligament and cartilage damage in more detail.
Is shoulder dislocation surgery risky?
Like any surgical procedure, shoulder dislocation surgery carries risks such as infection, bleeding, nerve injury, or anesthesia-related complications. However, today most of these surgeries are performed arthroscopically, meaning with minimally invasive techniques, which significantly reduces risks. The success of the surgery depends largely on the surgeon’s experience and your adherence to post-operative physical therapy. In recurrent dislocations, surgery is a highly successful and often necessary method to improve quality of life.