Reverse shoulder arthroplasty is a special arthroplasty technique in which the normal anatomical structure of the shoulder joint is deliberately reversed. In this surgical method, the ball that normally sits at the end of the arm bone (humerus) is mounted onto the scapula, while the socket on the scapula is placed on the upper end of the arm bone. Thanks to this ingenious mechanical change, reverse shoulder arthroplasty aims to restore shoulder function, especially in patients with irreparably damaged rotator cuff muscles who cannot lift their arm. Essentially, it transfers the function of the nonfunctional muscles to the deltoid muscle, the strongest muscle of the shoulder, creating a painless and functional joint.
| Indications |
– Advanced rotator cuff tear- Severe shoulder arthritis- Need for revision surgery- Functional loss after proximal humerus fracture
|
| Contraindications |
– Active infection- Absence of functional deltoid muscle- Severe neurological disorders- Severe vascular insufficiency
|
| Surgical Procedure |
– General or regional anesthesia is applied- The shoulder joint is accessed via posterior or deltopectoral approach- The humeral head is removed, the glenoid base is prepared and prosthesis is placed- The humeral part of the prosthesis is inserted and the prosthetic joint is created
|
| Advantages |
– Significant pain reduction- Increase in functional range of motion- Preservation of shoulder movement even in rotator cuff tears
|
| Disadvantages |
– A different movement pattern from normal shoulder biomechanics- Risk of implant loosening in the long term- Need for activity restrictions
|
| Possible Complications |
– Infection- Shoulder dislocation- Nerve injuries- Loosening or fracture of the prosthesis- Hematoma, seroma formation
|
| Rehabilitation |
– Passive movements start in the early period- Active movements after 4-6 weeks- Return to daily life at 3 months
|
| Long-Term Follow-up | – Radiological controls- Functional evaluation- Monitoring of complications |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What is reverse shoulder arthroplasty and what does its difference from a normal prosthesis mean?
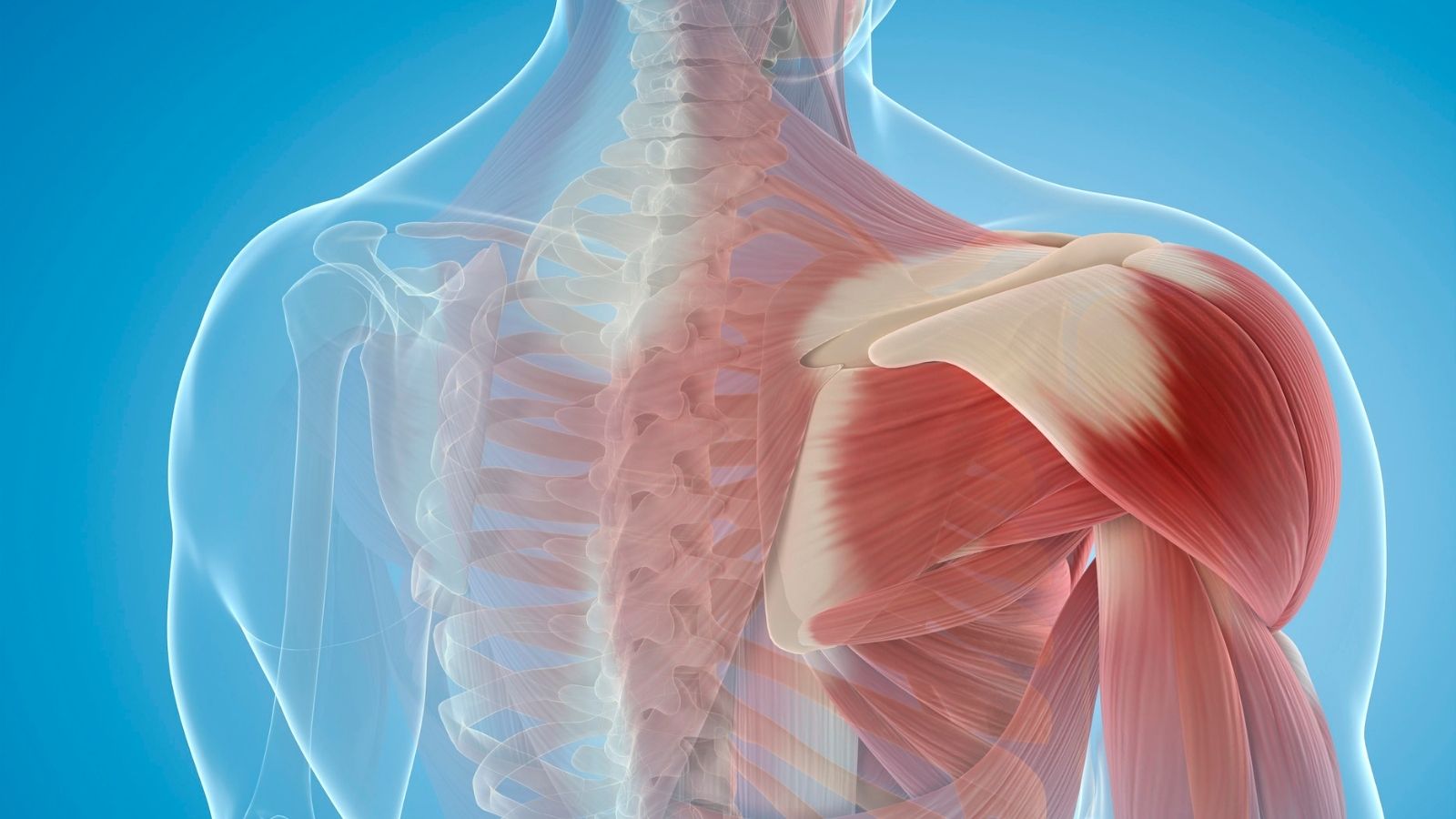
We can think of the shoulder joint as a simple mechanism: a ball and a socket. The head of our upper arm bone (humerus) acts as a ball and fits into a shallow socket (glenoid) on our scapula. The most important structure that holds this joint together and provides the incredible range of motion of our arm is a group of muscles and tendons called the “rotator cuff.” These muscles not only allow us to lift and rotate our arm but also stabilize the ball within the socket during movement.
So, what happens if these stabilizing muscles become completely dysfunctional due to long-term wear or severe trauma? In such cases, the shoulder mechanics are disrupted. When attempting to lift the arm, the deltoid muscle, the strongest shoulder muscle located on the outer side of the shoulder, pushes the ball uncontrollably upward instead of rotating it within the socket. This leads to unbearable pain and a condition called “pseudoparalysis,” where the person cannot actively raise their arm. For these patients, a normal (anatomical) shoulder prosthesis is not a solution, because anatomical prostheses mimic the natural shoulder and require an intact rotator cuff to function.
This is where reverse shoulder arthroplasty comes into play and solves the problem from a completely different perspective. Instead of imitating the anatomy, this prosthesis recreates the shoulder’s mechanics. The basic principle is to change the joint’s center of rotation so that the deltoid muscle becomes the primary mover in lifting the arm. It achieves this with two fundamental changes:
The Ball and Socket Switch Places: A metal ball (glenosphere) is placed on the scapular socket, while a polyethylene socket designed to perfectly fit this ball is attached to the top of the humerus.
The Deltoid Muscle Takes the Lead: The joint’s center of rotation is shifted inward and downward. This mechanical adjustment changes the pulling angle of the deltoid muscle. Instead of pushing the ball upward uncontrollably, the deltoid now efficiently rotates and lifts the arm around the new stable ball. The semi-constrained structure of the prosthesis provides additional stability and prevents unwanted upward movement.
In summary, while an anatomical shoulder prosthesis aims to “repair” a joint with intact muscles but damaged cartilage, a reverse shoulder prosthesis seeks to “create a new functional system” in a shoulder with failed muscles. This allows patients who could not previously use their arm to regain function and independence.
Who are candidates for reverse shoulder arthroplasty?
Reverse shoulder arthroplasty is not suitable for every shoulder pain. The most critical step for a successful outcome is proper patient selection. The main conditions where this surgery can significantly improve quality of life include:
- Advanced arthritis due to rotator cuff tear (Cuff Tear Arthropathy)
- Complex shoulder fractures in elderly patients that cannot be treated by other methods
- Failed previous shoulder prosthesis or fracture surgeries
- Inability to lift the arm due to massive cuff tear, even without arthritis (pseudoparalysis)
- Severe bone loss in the glenoid preventing anatomical prosthesis application
- Severe damage to both muscles and the joint due to conditions like rheumatoid arthritis
- Restoring function and filling the gap after tumor resection in the shoulder region
Additionally, certain basic requirements must be met for this surgery to be performed. The success of this operation depends entirely on a functioning deltoid muscle. Therefore, permanent damage to the deltoid muscle or the axillary nerve that activates it is an absolute contraindication. Likewise, sufficient healthy bone is required to securely fix the prosthesis component into the scapula. The presence of an active infection in the body or shoulder is also an absolute contraindication, as in all prosthetic surgeries.
What are the differences between various reverse shoulder prosthesis designs?
The first version of the reverse shoulder prosthesis (Grammont style) was revolutionary in shoulder surgery but over time showed certain shortcomings. The most well-known issues with this design were “scapular notching” (bone erosion at the scapula edge due to implant contact) and significant limitation in external rotation of the arm. The desire to overcome these limitations led to continuous improvements in prosthesis design.
Modern designs can broadly be understood under two philosophies: Medialized and Lateralized systems. This is like choosing between different car models—each has unique strengths and potential drawbacks, and the choice depends on patient needs.
- Classic Medialized Design (Traditional Approach):
This original design aimed to reduce shear forces on the glenoid base plate by shifting the joint’s center of rotation medially. It provides stable fixation, especially in patients with poor bone quality and higher loosening risk. Like a heavy-duty truck, it prioritizes stability and durability. However, it comes with drawbacks: higher risk of scapular notching and limited rotational movements.
- Modern Lateralized Designs (Innovative Approach):
These newer designs aim to address the shortcomings of the classic style by shifting the joint center slightly outward (laterally). This creates clearance to reduce notching and improves soft tissue tension, allowing significantly better rotational movement, especially external rotation. Like a sports car, these designs offer greater mobility. However, lateralization also increases mechanical stress on screws and may slightly raise the risk of loosening or acromial stress fractures.
Ultimately, there is no single “best” design. Surgeons tailor the choice to the patient’s age, bone quality, activity expectations, and anatomy, much like a custom-made suit. A medialized design may be better for frail bones, while lateralized systems can optimize motion in younger, active patients.
Contact us for detailed information and an appointment!
How will my life change after reverse shoulder arthroplasty, and what should I expect?
The most immediate and noticeable change for a patient undergoing reverse shoulder arthroplasty is usually the elimination of chronic pain that may have persisted for years. Many patients report that postoperative surgical pain feels much lighter compared to the unbearable arthritic pain they experienced before surgery. This dramatic pain relief alone significantly improves quality of life.
Besides pain relief, regaining function is the greatest benefit. For someone who previously could not bring a glass to their mouth, comb their hair, or reach an item on a shelf, being able to lift their arm to shoulder level again means regaining independence. This is the primary goal of the surgery: enabling the patient to perform daily activities comfortably and without pain.
However, maintaining realistic expectations is key to patient satisfaction. While reverse shoulder arthroplasty provides remarkable improvements, it does not restore the shoulder to a “brand-new” original state. It is a functional restoration surgery. Therefore, it is important to understand that some permanent limitations will remain after surgery. Critical points include:
- Avoid lifting loads heavier than 10–15 kilograms for life
- Avoid strenuous, high-impact tasks such as chopping wood or heavy gardening
- Competitive overhead sports such as tennis or volleyball are generally not possible
- Internal rotation (moving the arm behind the back) is usually the most limited motion
- Avoid using the operated arm to push yourself up from a chair or sofa
Even patients with a history of failed shoulder surgeries (such as unsuccessful rotator cuff repair) generally achieve excellent outcomes. Scientific studies show that although results in such cases may be slightly lower than in first-time surgeries, this difference is rarely perceptible to the patient. In other words, even with prior failed surgery, reverse shoulder arthroplasty can still provide life-changing benefits.
What are the possible risks of reverse shoulder arthroplasty?
Like any surgical procedure, reverse shoulder arthroplasty carries specific risks. It is a technically demanding surgery, and complication rates are slightly higher compared to standard shoulder prostheses. However, with an experienced surgeon and proper patient selection, these risks can be minimized. Awareness of possible risks helps patients better understand the process. Potential complications include:
- Prosthetic Dislocation (Instability): One of the most common early complications, often occurring when the arm is placed in a specific combined position (backward, sideways, and inward).
- Infection: The most feared complication in all joint replacements. In the shoulder, it may develop insidiously due to a slow-growing bacterium called Cutibacterium acnes, commonly found on the skin.
- Scapular Notching: Caused by prosthesis contact with the scapula. Modern prosthetic designs have greatly reduced this risk.
- Prosthesis Loosening: Over years, the prosthesis may lose fixation to bone even without infection. This is the most common late failure cause.
- Stress Fractures in Shoulder Bones: Particularly in the acromion due to increased deltoid tension.
- Intraoperative Fractures: May occur in patients with very poor bone quality during bone preparation or prosthesis placement.
- Nerve Injury: Risk of temporary or, rarely, permanent damage to nerves near the surgical field.
- Blood Clot Formation (Deep Vein Thrombosis): As with all major surgeries, there is a risk of clots forming in the legs or lungs.
Although this list may look intimidating, it is important to remember that the majority of these complications are rare. Your surgeon will assess your personal risk factors (age, bone quality, other health conditions, etc.) and take the necessary precautions. For example, in patients at higher risk of dislocation, soft tissue balancing may be adjusted differently, or in patients with higher infection risk, additional antibiotic measures may be applied. The process is a team effort, and you are an important member of that team.
How does rehabilitation and physiotherapy progress after reverse shoulder arthroplasty?
The success of reverse shoulder arthroplasty does not end at the operating room door—it begins there. Postoperative rehabilitation and physiotherapy are just as crucial as the surgery itself and differ significantly from conventional shoulder prosthesis rehabilitation. The core principle here is “do not rush” and “protect.” The goal is to give the prosthesis and the deltoid muscle, now the main mover, enough time to adapt to the new mechanics. The process is divided into phases, with progression based not only on time but also on achieving specific goals.
- Phase 1: Maximum Protection (First 6 weeks)
The sole priority is protecting the healing tissues and the new prosthesis.
Your arm is kept in a special sling with pillow support.
The sling must remain in place at all times, including while sleeping, except during bathing and exercises shown by your therapist.
Self-initiated shoulder movements using your own muscle power are strictly prohibited during this phase.
Only gentle “passive” movements, performed with the help of the other arm or guided by a physiotherapist, are allowed.
Elbow, wrist, and finger exercises are encouraged to promote circulation and prevent stiffness.
- Phase 2: Transition to Active Motion (Typically 6–12 weeks)
At this stage, shoulder muscles are gradually reactivated.
You may start removing the sling during the day.
Assisted-active exercises are introduced, such as moving the operated arm with the help of a stick or the other arm.
Gentle isometric exercises may begin to prevent muscle atrophy.
Lifting anything heavier than a coffee cup is still prohibited.
- Phase 3: Strengthening (After 12 weeks)
This is when confidence returns and functional recovery advances.
From about the 12th week, you begin performing fully active, unsupported arm movements.
Strengthening exercises are introduced, starting with very light weights (0.5–1 kg) and gradually increasing over time.
The focus shifts from the now nonfunctional rotator cuff muscles to the deltoid and supporting scapular muscles.
Throughout this period, lifelong rules must be remembered: avoid combined movements of backward, sideways, and inward rotation, as well as pushing yourself up with the operated arm, to prolong prosthesis lifespan and prevent dislocations. Patience, discipline, and collaboration with your physiotherapist are essential to success.
What does the future hold for reverse shoulder arthroplasty technology?
In the past two decades, reverse shoulder arthroplasty has advanced greatly with new implant designs. However, the future focus is not just on making better implants, but on tailoring them to each patient’s unique anatomy with maximum precision. Exciting developments in surgical planning and operating room technology include:
- 3D Surgical Planning: Instead of relying on standard X-rays, surgeons now use 3D virtual models from CT scans. This allows precise analysis of bone anatomy and angles, testing of implant sizes, and planning of screw positioning before surgery.
- Patient-Specific Surgical Guides (PSI): Using 3D printing, personalized surgical guides are created to match each patient’s anatomy, guiding drills and implants exactly as planned.
- Robotic-Assisted Systems: Borrowed from hip and knee surgery, robotic systems enhance surgical precision. The robot does not operate independently but assists the surgeon by guiding instruments according to the preoperative 3D plan.
- Augmented Reality Glasses: Surgeons can overlay 3D surgical plans directly onto the patient’s anatomy in real time, improving accuracy during critical steps like implant positioning.
- AI-Based Outcome Prediction: Artificial intelligence trained on large datasets can predict postoperative range of motion and pain relief tailored to each patient’s age, bone quality, and activity level, improving decision-making and managing expectations.
Contact us for detailed information and an appointment!