Prof. Dr. Murat Demirel, one of the best orthopedic doctors performing hip dislocation surgery in Ankara, is a trusted name with many years of experience in treating congenital (developmental) or trauma-related hip dislocations. Hip dislocation is a serious orthopedic problem that can lead to joint incongruity, difficulty walking, and permanent joint damage. Among the hospitals performing hip dislocation surgery in Ankara, Prof. Dr. Demirel applies personalized surgical plans for each patient in advanced medical facilities with high hygiene standards.
By conducting detailed evaluations before surgery, Prof. Dr. Demirel determines the most appropriate surgical technique and closely monitors his patients after the operation. With his post-operative recommendations, the recovery process after hip dislocation surgery is ensured to be fast, safe, and permanent. In addition, by providing transparent and up-to-date information about hip dislocation surgery costs in Ankara, he helps his patients make informed decisions. You can also book an appointment immediately to protect your hip health, reduce your pain, and increase your mobility.
| Disease Name | Hip Dislocation (in Adults) |
| Affected Area | Hip joint (femoral head and acetabulum) |
| Symptoms | Severe hip pain, leg shortening, limited movement, external or internal rotation of the leg |
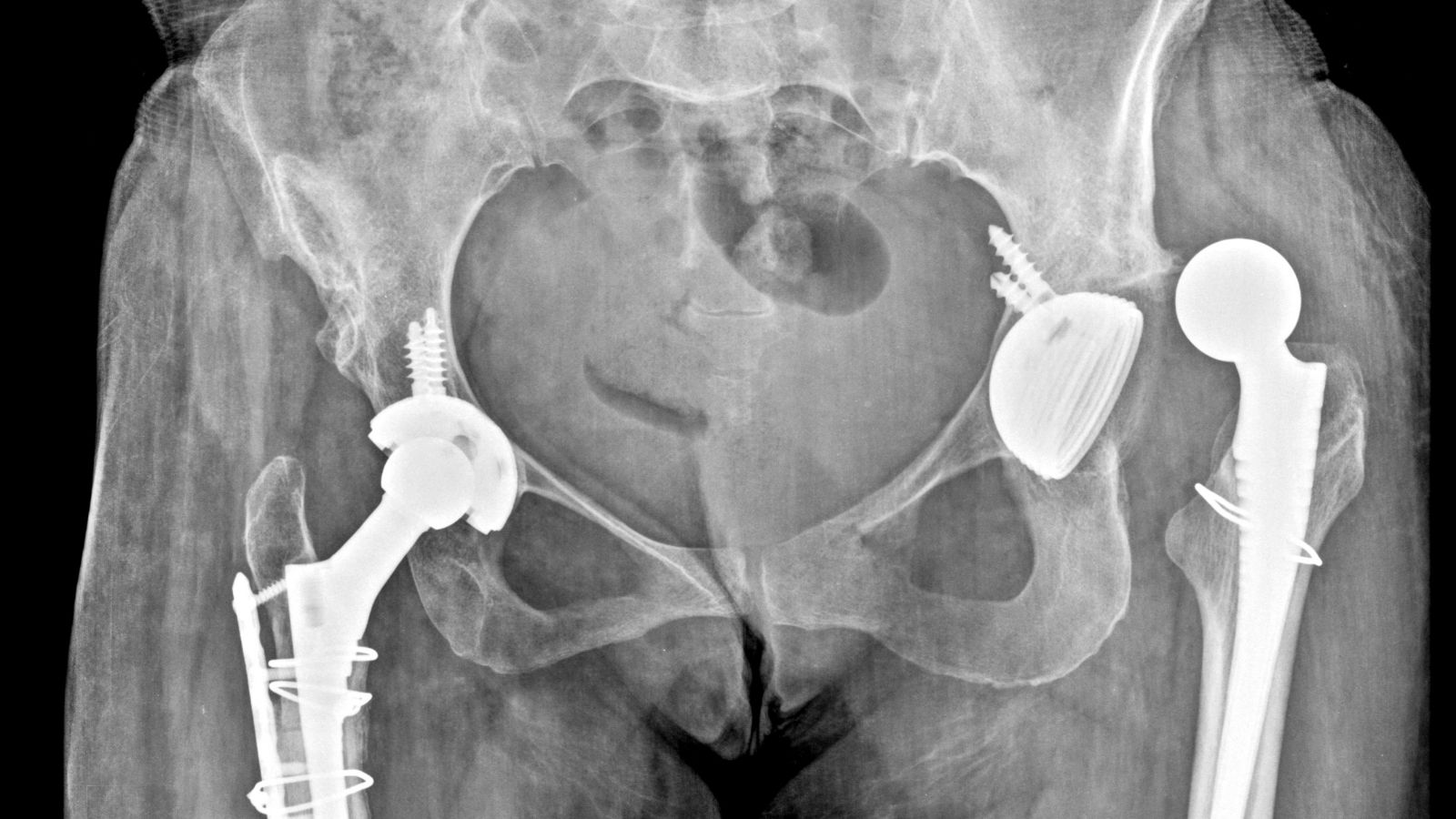
| Diagnostic Methods | Physical examination, X-ray, CT |
| Causes | Trauma (traffic accident, fall), less commonly deformity caused by developmental hip dysplasia in adulthood |
| Risk Factors | Severe trauma, history of hip prosthesis, hip dysplasia, ligament laxity |
| Treatment Methods | Closed reduction, open reduction, rehabilitation, surgical stabilization in recurrent dislocations |
| Surgical Options | Open reduction, acetabular reshaping, hip replacement (in late-stage osteoarthritis) |
| Complications | Avascular necrosis of the femoral head, recurrent dislocation, nerve injuries (especially sciatic nerve), hip arthritis |
| Recovery Process | 6–12 weeks; varies depending on physical therapy and loading protocol |
| Prevention Methods | Protection from trauma, in-vehicle safety precautions, early diagnosis and treatment |
| Follow-up Process | Radiological checks, physical therapy evaluations, long-term complication follow-up |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What is Hip Dislocation and What Types Exist?
We evaluate hip dislocation in different categories based on the cause of occurrence and the age group in which it is seen. This distinction is very important because each condition has its own story, treatment approach, and follow-up process. The situation of a young patient who has had a traffic accident is completely different from a newborn baby with a developmental problem in the hip.
To better understand hip dislocations, we can divide them into main groups:
- Traumatic Hip Dislocation
- Developmental Hip Dislocation (DDH)
- Dislocation After Total Hip Prosthesis
These three main categories form the basis of the hip dislocation spectrum. Traumatic dislocations are usually the subject of emergency rooms and trauma centers, while DDH is one of the most important areas of pediatric orthopedics. Post-prosthetic dislocations appear as a potential complication of hip replacement surgery. The management path for each has a profound impact on the patient’s future joint health and quality of life, which is why correct diagnosis and classification are the first and most critical steps of treatment.
Under What Circumstances Does a Traumatic Hip Dislocation Occur?
As the name suggests, traumatic hip dislocation occurs when the body is exposed to a high-energy force. The hip joint is such a strong structure that it takes tremendous force to dislocate it. This type of injury usually occurs not during the normal flow of life but during unexpected and severe events.
The most common scenarios leading to this condition are:
- Motor vehicle accidents
- Falls from height
- Severe industrial or workplace accidents
- Violent collisions in contact sports (American football, rugby, skiing, etc.)
Especially in traffic accidents, the classic mechanism is when a seated person’s knee hits the car dashboard violently. This impact travels like a shockwave along the thigh bone, pushing the head of the femur backward out of its socket, causing dislocation. For this reason, this injury is also called a “dashboard injury.”
It is important to remember that such a severe trauma rarely affects only the hip. The entire body is impacted by this energy. Therefore, when evaluating a patient with a hip dislocation, we always look for accompanying injuries. These may include additional fractures in the pelvis, knee, or other leg bones, as well as abdominal, chest, or head trauma. That is why a patient with a hip dislocation is always considered a polytrauma patient and all body systems are carefully examined.
What Are the Most Common Symptoms of Hip Dislocation?
When a hip dislocation occurs, the body gives very clear and strong signals. These symptoms are so obvious that it is almost impossible for the person to ignore them or think they will simply go away. The warning signs that should never be ignored are:
- Unbearable, stabbing severe pain
- Inability to move the affected leg
- Leg locked in an abnormal and awkward position
- The affected leg appearing shorter than the other
- Visible swelling or deformity in the hip area
- Hearing or feeling a “pop,” “click,” or similar cracking sound in the hip at the time of injury
- Numbness, tingling, or pins-and-needles sensation in the foot or ankle
- Difficulty or complete inability in lifting the foot upward (dorsiflexion), also known as foot drop
Especially the position of the leg provides an important clue for us doctors. In posterior dislocations, the leg is usually inwardly rotated and bent, whereas in anterior dislocations, it is often positioned outwardly. Symptoms such as numbness and weakness may indicate that the sciatic nerve, the major nerve running right behind the hip, is under pressure. This is a critical finding that further increases the urgency of treatment.
Contact us for detailed information and an appointment!
How is Hip Dislocation Diagnosed?
When a patient arrives at the emergency room with suspected hip dislocation, it triggers a process where the entire team quickly takes action. Diagnosis is made by combining the patient’s history, physical examination findings, and imaging tests. This process requires careful, step-by-step evaluation.
Initial Evaluation and Physical Examination: Everything starts with listening to the patient and understanding how the injury occurred. Then, a comprehensive physical examination is performed. The leg’s resting position, whether there is a length difference, and deformity in the hip area are carefully checked. One of the most critical parts of this examination is the neurovascular assessment. This means checking the blood circulation in the leg (pulses) and testing the nerve functions (sensation and muscle strength). Detecting possible vascular or nerve damage early is vital.
Imaging Methods: To confirm suspicions from the physical exam and to reveal all the details of the injury, imaging tests are used. These tests provide us with a roadmap for treatment planning.
We can summarize what imaging tests tell us as follows:
X-ray: The first and most basic step that confirms the diagnosis. It clearly shows the presence and direction of the dislocation (anterior or posterior). It also helps detect large and obvious fractures.
Computed Tomography (CT): An indispensable tool in managing hip dislocation. It is especially requested after the hip has been relocated to ensure that everything in the joint is in order. CT shows in three dimensions the smallest bone fragments, fractures in the acetabular walls, and joint congruity that might be missed on an X-ray. CT findings play a critical role in deciding whether the next step in treatment should be surgery.
How is Developmental Hip Dislocation in Babies Recognized?
Developmental Dysplasia of the Hip (DDH) is a completely different entity from traumatic dislocations. Instead of a sudden injury, this condition involves a developmental defect of the hip joint beginning in the womb. While it can be concerning for parents, understanding and detecting it early is the key to successful treatment. DDH occurs when the hip socket is too shallow for the femoral head to remain stable in the socket. This can range from mild looseness to a complete dislocation.
Who is at Risk for DDH?
Some babies have a higher likelihood of developing DDH than others. The risk factors include:
- Family history of DDH
- Being female
- Being the first child in the family
- Breech presentation in the womb
- Low amniotic fluid during pregnancy (oligohydramnios)
- Tight swaddling that keeps the legs straight and together
What Signs Should Parents Watch Out For?
While routine doctor check-ups are crucial for detecting this condition, there are also some clues that parents may observe at home. Remember, hip dislocation in babies does not cause pain, so the signs are mostly visual or movement-related:
- Asymmetry in the number or placement of skin folds on the thighs
- One leg appearing shorter than the other
- Restriction in hip abduction, with one leg opening less than the other
- A “click” or “pop” sound when changing the baby’s diaper
- Limping when the child starts walking
- Waddling gait if both hips are affected
Diagnosis and Screening Process
In our country, all newborns are screened for DDH. During the first months after birth, doctors perform special maneuvers (Ortolani and Barlow tests) to check the stability of the hip. In cases of suspicion or risk factors, the most reliable diagnostic method within the first 4–6 months is hip ultrasound. Ultrasound provides the best view of the cartilage structures of the still-developing hip joint. For babies older than 6 months, X-ray is preferred. Early diagnosis allows simple and effective treatment with devices such as the Pavlik harness, ensuring the child has healthy hips in the future.
Why is Emergency Intervention in Hip Dislocation So Important?
The definition of “orthopedic emergency” means that the situation is not only painful but also time-sensitive to prevent permanent damage. Hip dislocation is one of the most important examples of this. From the moment of diagnosis, the goal is to reduce the dislocation within the first 6 hours. Behind this urgency are two major irreversible dangers.
The first and most critical risk is Avascular Necrosis (AVN). The spherical head of the femur is supplied by very delicate blood vessels. When the hip dislocates, these vessels can stretch, kink, or rupture. If blood flow is cut off, the bone tissue literally “dies.” This leads to collapse of the femoral head, damage to the joint surface, and severe progressive arthritis. Ultimately, this often results in the need for a total hip replacement at a young age. Every hour the hip remains dislocated increases the risk of this devastating complication.
The second major danger is permanent nerve damage. Especially in posterior dislocations, the displaced femoral head directly compresses the sciatic nerve, which controls almost all motor and sensory functions of the leg. The longer this pressure lasts, the greater the risk of permanent damage to nerve cells. This can lead to foot drop, lasting weakness, loss of sensation, and lifelong chronic neuropathic pain (sciatica).
For these reasons, intervention in hip dislocation is not just about “putting it back in place” but a race against time to save the future of the joint and the nerve.
Are There Non-Surgical Treatment Options for Hip Dislocation?
Yes, many hip dislocations, especially when addressed promptly, can be successfully treated without surgery. The cornerstone and first step of non-surgical treatment is called “closed reduction.”
Closed reduction involves manipulating the femoral head back into its socket using controlled pulling and rotating maneuvers, without any surgical incision. Because this procedure is quite painful, it is always performed under general anesthesia or deep sedation in a fully equipped setting like an operating room or emergency department. The physician takes advantage of muscle relaxation to perform gentle maneuvers that minimize joint damage.
The main non-surgical approaches depending on the type of dislocation are:
Traumatic Hip Dislocation: Managed with closed reduction.
Developmental Dysplasia of the Hip (First 6 Months): Managed with a Pavlik harness, a special brace system.
Dislocation After Total Hip Prosthesis: Initially, closed reduction is attempted.
When successful, the physician typically feels a distinctive “click” as the femoral head slips back into place. Afterwards, control X-rays or often a CT scan are performed to confirm success and rule out additional intra-articular problems. To allow healing of injured ligaments and capsule, the patient may need to use crutches for a period and avoid specific hip movements.
When Does Hip Dislocation Surgery Become Necessary?
Although closed reduction is the first choice, it is not always possible or sufficient. In some cases, surgical intervention becomes inevitable to restore joint health and stability. The main situations that necessitate surgery include:
- Failure of closed reduction attempts
- Bone or soft tissue fragments trapped inside the joint
- Incongruity in the joint seen on CT after reduction
- Accompanying acetabular fracture compromising stability
- Fracture of the femoral head or neck
- Persistent instability even after reduction
- Delayed presentation after injury
In such cases, different surgical methods are applied depending on the problem. In open reduction, the surgeon makes an incision to access the joint, removes trapped fragments, and places the femoral head directly back into the socket under visual control. If there is an accompanying fracture, Open Reduction and Internal Fixation (ORIF) is performed with plates or screws. In some cases, especially for intra-articular cartilage or labrum injuries, minimally invasive hip arthroscopy can be used. The choice of surgery depends on the characteristics of the injury and is tailored to each patient.
What Risks and Complications May Develop After Hip Dislocation?
Even after treatment, hip dislocation carries potential risks that may affect the patient’s life long-term. These complications vary depending on the severity of the initial injury and the timeliness of treatment. Being informed about these risks helps patients understand the importance of follow-up.
The most common potential complications include:
Avascular Necrosis (AVN): Loss of blood supply and death of the femoral head.
Post-traumatic Arthritis: Degenerative changes in the joint after injury.
Permanent Nerve Damage: Especially involving the sciatic nerve.
Recurrent Dislocations (Chronic Instability): The hip repeatedly slipping out of place.
Heterotopic Ossification: Abnormal bone formation in soft tissues.
Blood Clots (Deep Vein Thrombosis / Pulmonary Embolism): Risk of clots forming due to post-surgical immobility.
It is important to understand that these complications are often interrelated. For example, AVN can directly lead to post-traumatic arthritis. Severe arthritis may eventually require total hip replacement. Nerve injury can cause weakness and abnormal gait, leading to faster joint wear. This domino effect shows why initial injury management must be taken so seriously. Long-term follow-up is critical for early detection and management of complications.
How Does the Recovery and Rehabilitation Process Progress After Hip Dislocation?
Recovery after hip dislocation is like running a marathon; it is a long process requiring patience, discipline, and professional support. Full functional recovery usually takes several months, with physical therapy and rehabilitation playing a central role. The goal is not only to wait for the joint to heal but also to safely restore lost functions.
The rehabilitation program is typically divided into phases, each with specific goals:
Phase 1: Early Stage (Approx. 0–6 Weeks) – Protection and Control
The aim is to protect the healing joint, control pain and swelling, and minimize muscle loss.
- Partial or no weight-bearing with crutches
- Avoiding restricted movements (e.g., deep squatting)
- Simple bed exercises
- Ankle pumps
- Isometric contractions without stressing the hip
Phase 2: Intermediate Stage (Approx. 6–12 Weeks) – Movement and Strengthening
Once the doctor confirms sufficient bone and soft tissue healing, rehabilitation moves to the next stage. The goal is to improve range of motion and begin strengthening.
- Non-resistance stationary cycling
- Aquatic therapy and exercises
- Light strengthening exercises under physiotherapist supervision
- Gait training to normalize walking
Phase 3: Advanced Stage (Approx. 3–6 Months) – Return to Function
The final stage aims to safely return the patient to daily activities and, if applicable, sports. Strength, endurance, balance, and coordination are maximized.
- More challenging balance exercises
- Functional movements (stair climbing, controlled squats)
- Beginning low-impact running (with doctor’s approval)
- Sport-specific training drills
Every patient’s recovery process is unique. Therefore, rehabilitation must always be tailored to the individual and closely monitored by an orthopedic specialist and physiotherapist.
Can Hip Dislocation Occur After Total Hip Replacement Surgery?
Yes, although total hip replacement is one of the most successful modern orthopedic procedures, it still carries risks. One of these is dislocation of the artificial joint after surgery. This rare but concerning complication is most likely to occur within the first 3 months after surgery, before surrounding muscles and ligaments adapt to the new joint.
Factors contributing to prosthetic dislocation include technical issues with component positioning, weakness of hip muscles, history of previous hip surgeries, or failure to adhere to post-operative movement restrictions.
When a prosthetic dislocation occurs for the first time, it can usually be treated successfully with closed reduction under anesthesia. However, recurrent dislocations often indicate a deeper issue. In such cases, revision surgery may be required, involving replacement of implant parts or use of more stable components. This is why strictly following post-operative precautions and physiotherapy guidance is critical to minimizing risk.
How to Manage Pain After Hip Dislocation Surgery?
Pain after hip dislocation surgery is a natural and expected part of recovery. The important thing is knowing that this pain is manageable. Effective pain management not only improves comfort but also accelerates recovery. A patient with well-controlled pain rests better, experiences less stress, and most importantly, can start physical therapy earlier and more willingly. Early mobilization reduces the risks of complications such as blood clots and infection.
Today, we use a modern approach called “multimodal analgesia” for pain control. Instead of relying on a single strong medication, this approach combines different methods that work through various mechanisms to provide more effective relief with fewer side effects.
Pain management strategies after surgery may include:
- Standard pain relievers (Paracetamol, anti-inflammatory drugs)
- Short-term controlled use of opioids for severe pain
- Regional nerve blocks applied during surgery
- Patient-controlled analgesia (PCA) pumps
- Regular application of ice packs to the surgical site
- Keeping the leg elevated above heart level
Successful pain management relies on open communication between the patient and healthcare team. Informing your medical team about changes in your pain levels and the adequacy of current treatment allows your pain plan to be customized and ensures a much more comfortable recovery process.
Contact us for detailed information and an appointment!
Frequently Asked Questions
What is hip dislocation in adults and how does it occur?
In adults, hip dislocation occurs when the head of the femur (thigh bone) completely or partially slips out of the hip socket (acetabulum). It usually develops due to untreated congenital hip dislocation, car accidents, falls from height, or severe trauma.
What symptoms does an adult with hip dislocation experience?
Adults with hip dislocation may experience severe hip pain, restricted movement, leg length discrepancy, limping, asymmetry in leg position, and sometimes outward rotation of the leg. In acute dislocations, movement may become almost impossible.
How is hip dislocation diagnosed?
Diagnosis begins with a detailed physical examination. Imaging methods such as X-ray, computed tomography (CT), or magnetic resonance imaging (MRI) are then used to confirm the condition. These tests also help assess any accompanying bone or soft tissue injuries.
What happens if hip dislocation is left untreated?
If left untreated, hip dislocation can cause permanent deformities in the joint, early arthritis, chronic limping, and persistent pain. Over time, the joint may suffer irreversible damage, leading to a significantly reduced quality of life.
How is hip dislocation treated in adults?
Treatment depends on the type of dislocation and the extent of joint damage. In recent dislocations, non-surgical closed reduction can reposition the bone. However, in most cases, surgical intervention such as open reduction, joint reconstruction, or hip replacement may be necessary.
What is the recovery process after hip dislocation surgery?
After surgery, patients are usually encouraged to walk with assistance in the first few days. Physiotherapy and rehabilitation play a crucial role. Recovery time varies depending on age, general health, and surgical technique, but most patients return to daily life within 2–3 months.
Can hip dislocation recur in adults?
Yes, hip dislocation may recur if it is not properly treated or if rehabilitation is insufficient. The risk is higher in patients with loose connective tissues or anatomical abnormalities.
What is the role of physiotherapy in treating hip dislocation?
Physiotherapy strengthens the muscles, improves joint stability, and speeds up recovery. Whether after surgery or non-surgical treatment, physiotherapy programs are essential for restoring mobility, reducing pain, and regaining normal walking function.
How is the return to daily life after hip dislocation?
With proper treatment and rehabilitation, most patients can resume their daily activities without problems. However, it is recommended to avoid heavy lifting, sudden movements, and activities with a high risk of falls. Regular check-ups and prescribed exercises are important for long-term success.
Are there non-surgical treatment options for hip dislocation in adults?
In acute, traumatic, and complete dislocations, surgery is usually necessary. However, in some chronic or mild cases, pain management, physiotherapy, the use of canes or walkers, and medications can improve quality of life. The appropriate treatment is determined by an orthopedic specialist based on the patient’s condition.