Prof. Dr. Murat Demirel, one of the best orthopedic doctors in Ankara specializing in hip osteoarthritis treatment, stands out with his many years of experience in treating this condition caused by cartilage wear and deformation on the joint surface over time. Hip osteoarthritis is a condition that restricts mobility, makes daily activities difficult, and seriously affects quality of life. Among the hospitals providing hip osteoarthritis treatment in Ankara, Prof. Dr. Demirel offers personalized treatment plans in centers equipped with advanced medical technology and high hygiene standards.
Depending on the stage of the disease, treatment options include medication, physical therapy, intra-articular injections, stem cell or PRP applications, and surgical methods when necessary. Following treatment, he ensures that his patients’ recovery process is fast, safe, and lasting by providing proper medical guidance. In addition, he offers transparent and up-to-date information about hip osteoarthritis treatment prices in Ankara, helping his patients make informed decisions. You can also schedule an appointment right away to protect your hip health, reduce pain, and improve your freedom of movement.
| Disease Name | Hip Osteoarthritis (Hip Arthritis) |
| Affected Area | Hip joint (acetabulum and femoral head) |
| Symptoms | Pain in the groin and hip, morning stiffness, limping, limited mobility, difficulty climbing stairs |
| Diagnosis Methods | Clinical examination, X-ray (narrowing of joint space, osteophytes), MRI |
| Causes | Cartilage degeneration, aging, post-trauma, hip dysplasia, avascular necrosis, rheumatic diseases |
| Risk Factors | Aging, obesity, joint trauma, hip deformities, genetic factors |
| Treatment Methods | Conservative: NSAIDs, physical therapy, exercise, use of cane, intra-articular injections (hyaluronic acid, PRP), Surgical: total hip replacement |
| Surgical Options | Total hip arthroplasty (hip replacement) |
| Complications | Decreased joint movement, increased pain, loss of function, complications after prosthesis |
| Recovery Process | Weeks to months with conservative treatment; 6–12 weeks after surgery |
| Prevention Methods | Weight control, strengthening of muscles, protection from joint injuries |
| Follow-Up Process | Radiological monitoring, symptom evaluation, rehabilitation follow-up |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What is Hip Osteoarthritis and What Happens in the Joint?
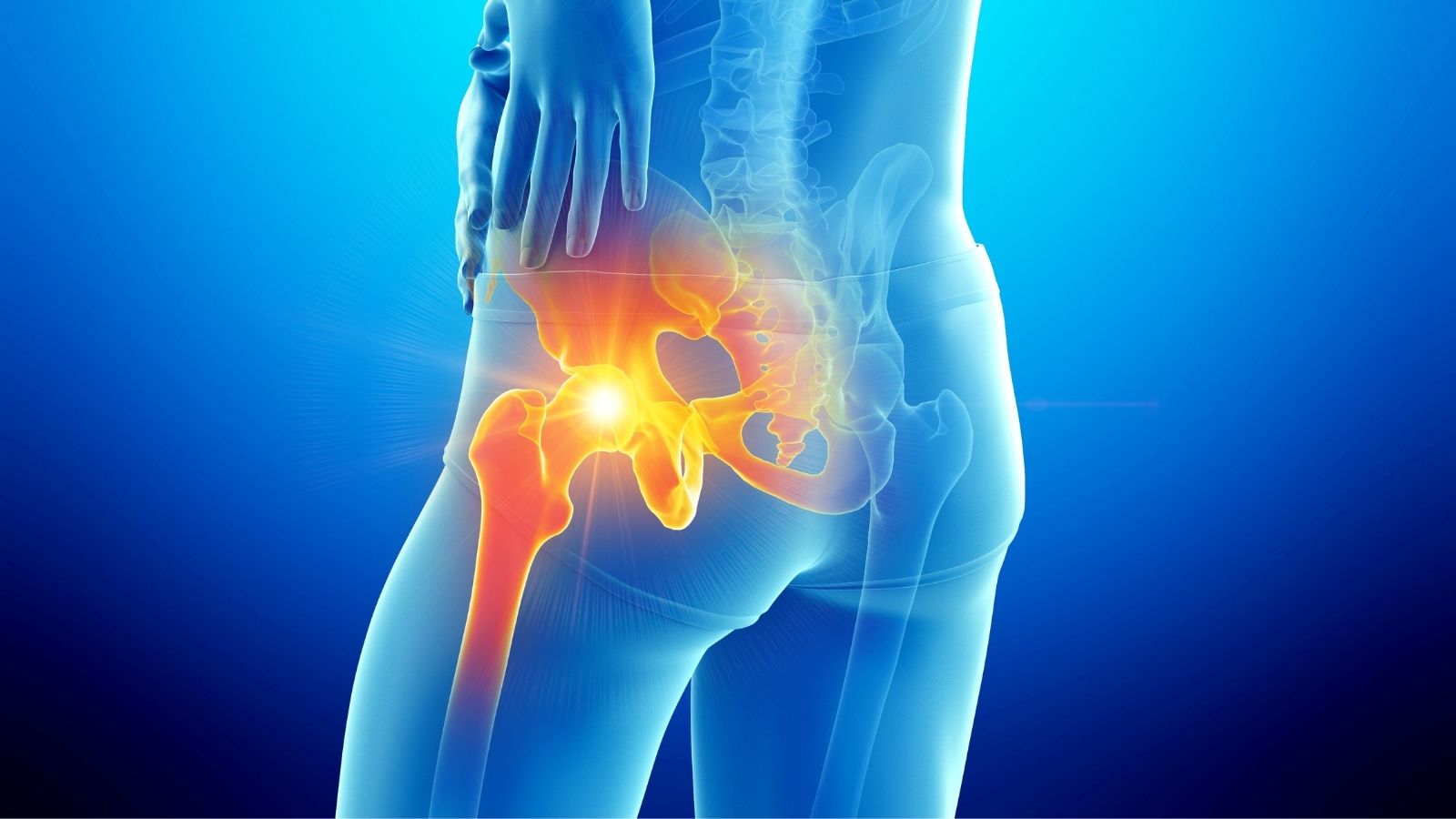
You can think of your hip joint like a hinge that allows a door to open and close perfectly. What makes this hinge work smoothly is the articular cartilage, a shiny, flexible, and slippery tissue that covers the ends of the bones. This cartilage also acts as a shock absorber, cushioning the load from body weight and preventing the bones from rubbing against each other.
So, what changes occur in this perfect structure when hip osteoarthritis begins? The process usually develops slowly and insidiously. Over time, due to various factors, this precious cartilage tissue begins to lose its water and elasticity. Its surface loses smoothness, cracks, and thins. Our body perceives this damage as a threat and initiates a repair mechanism. However, this attempt to repair can unfortunately complicate the situation further.
To support the weakening cartilage, the body thickens and hardens the underlying bone tissue. This is called “sclerosis.” At the same time, small, sharp bony projections called “osteophytes” begin to form at the edges of the joint. These outgrowths restrict the joint’s normal movement and cause catching sensations or even pain with each movement.
As the disease progresses, the cartilage can completely disappear. This is the most advanced stage, and the bone surfaces begin to rub directly against each other without protection. This leads to severe and persistent pain, obvious limping, and near-total loss of hip joint motion. As can be seen, hip osteoarthritis is much more than a simple “wear and tear” problem. It is an active disease affecting all components of the joint and involving the body’s complex biological responses.
Why Does Hip Osteoarthritis Occur and Who Is at Risk?
One of the most common questions my patients ask during examination is, “Doctor, why did this happen to me?” Hip osteoarthritis does not have a single cause. It usually develops from the combination of multiple factors, like pieces of a puzzle. Sometimes we cannot find any underlying cause, which is called “primary osteoarthritis.” Sometimes there is another condition that triggers osteoarthritis, which is called “secondary osteoarthritis.”
Factors and conditions that increase the risk of hip osteoarthritis include:
- Advancing age
- Family history (genetic predisposition)
- Excess weight (obesity)
- Previous hip injuries
- Hip fractures or dislocations
- Congenital hip dislocation (developmental hip dysplasia)
- Hip impingement syndrome
- Avascular necrosis (impaired blood supply to the femoral head)
- Certain rheumatic diseases
- Occupations requiring repetitive heavy lifting
- High-impact professional sports
Having one or more of these factors does not mean you will definitely develop hip osteoarthritis. However, knowing that they increase risk is important for taking precautions and seeking early diagnosis. Remember, hip osteoarthritis can also occur in people without any of these risk factors.
What Are the Most Typical Symptoms of Hip Osteoarthritis?
Hip osteoarthritis usually manifests gradually. Initially mild and often disregarded complaints can, over time, turn into problems that seriously impact daily life. Recognizing these symptoms early is crucial for beginning treatment sooner and slowing disease progression.
The most common symptoms of hip osteoarthritis include:
- Groin pain
- Pain on the outer side of the hip
- Pain in the front of the thigh
- Pain radiating to the knee (sometimes mistaken for a knee problem)
- Pain that worsens with activity and improves with rest
- Stiffness after waking up or after prolonged sitting
- Reduced walking distance
- Limping
- Difficulty climbing up and down stairs
- Difficulty putting on socks or shoes
- Difficulty getting in and out of a car
- Clicking or grinding sounds from the joint
- Weakness and fatigue in the hip muscles
If you are experiencing one or more of these symptoms, it is best to consult an orthopedic and traumatology specialist without underestimating the condition.
Contact us for detailed information and an appointment!
What to Expect at the Doctor’s Visit for Hip Osteoarthritis Diagnosis?
When you consult a doctor with the suspicion of “Do I also have hip osteoarthritis?”, a systematic process is followed to reach a diagnosis. This process begins with a detailed conversation with you and usually concludes with simple imaging methods. There is no need to worry; the process is quite straightforward.
First, we talk with you and listen to the story of your complaints. This is the most valuable information for us. We try to understand your problem by asking questions such as: How long have you had pain, where do you feel it, at what times of the day or with which movements does it worsen, what activities does it prevent you from doing, have you tried any treatment before? Your family history, occupation, lifestyle, and other health problems also provide us with important clues.
Next comes the physical examination. This is one of the most critical steps in the diagnosis. We observe you walking to detect any limping. On the examination table, we assess the movements of your hip. By moving your leg in different directions (bending, straightening, abduction, internal and external rotation), we both measure your range of motion and determine which movements cause pain. Limited internal rotation of the hip is a very typical finding for hip osteoarthritis. We also check the strength of the muscles around the hip.
Usually, patient history and physical examination findings give us a strong idea about the diagnosis. To confirm this idea and determine the stage of the disease, we use imaging methods. The first and most common method is X-ray. A simple standing hip X-ray clearly shows whether there is narrowing of the joint space, the presence of bony outgrowths (osteophytes), and other changes in bone structure. In most cases, X-ray is sufficient for diagnosis. Advanced imaging methods such as Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) are not always necessary. We use these methods more when the diagnosis is uncertain, when we suspect another condition accompanying osteoarthritis (such as cartilage tear, bone marrow edema, avascular necrosis), or when we are planning surgical treatment and need to see the joint in detail in three dimensions.
How Is Hip Osteoarthritis Treated Without Surgery?
When you are diagnosed with hip osteoarthritis, you don’t need to immediately think of the worst-case scenario. Especially in the early and moderate stages, there are many effective treatments that can control pain and improve your quality of life without surgery. Remember, the main goal of these treatments is not to restore the lost cartilage (this is not yet possible), but to manage the current condition, relieve pain, and slow disease progression. The treatment plan is tailored specifically for you, depending on your lifestyle, expectations, and the stage of the disease.
Lifestyle Changes: The Cornerstone of Treatment
This is the most important part of treatment and is entirely under your control. Reaching or maintaining your ideal weight is the best thing you can do. Every 1 kilogram of weight loss reduces the load on your hip joint by 4–6 kilograms. This can make a significant difference in your pain. It is also very important to regulate your activities. You should avoid activities that put impact stress on your joint.
Recommended low-impact activities include:
- Swimming
- Water exercises (aqua gym)
- Cycling (with low resistance and correct saddle adjustment)
- Elliptical trainer
- Walking (on soft, flat ground, with supportive shoes)
- Pilates (modified and with professional supervision)
- Yoga (avoiding strenuous poses)
High-impact activities to avoid or limit:
- Running (especially on hard surfaces like concrete)
- Jumping sports (basketball, volleyball, tennis)
- Movements involving heavy weights such as squats
- Football
Physical Therapy and Rehabilitation
Physical therapy is an essential part of hip osteoarthritis management. With a personalized exercise program prepared under the guidance of a physiotherapist, the muscles around the hip, waist, and abdomen are strengthened. Strong muscles act as a natural corset for the joint, reducing load, increasing balance, and alleviating pain. Stretching exercises also help maintain and improve joint mobility.
Medications and Intra-Articular Injections
During periods of intense pain, medications can be used. Simple painkillers such as paracetamol may be the first choice. When these are insufficient, non-steroidal anti-inflammatory drugs (NSAIDs), which both relieve pain and reduce inflammation in the joint, can be prescribed. However, it is important to use these medications under medical supervision due to possible stomach and kidney side effects.
When medications are insufficient or cannot be used, injections directly into the hip joint may be considered. The most commonly used include:
- Corticosteroid injections
- Hyaluronic acid injections (joint fluid supplementation)
- PRP (Platelet-Rich Plasma) injections
- Stem cell therapies
Each of these injections has different mechanisms of action and success rates. The most suitable method for you is decided together, based on the stage of the disease and your overall health condition.
When Does Surgical Treatment Become Necessary in Hip Osteoarthritis?
Surgery is usually the final step in hip osteoarthritis treatment. However, this does not mean “last resort” or “failure.” On the contrary, when performed at the right time on the right patient, it is a highly successful solution that dramatically improves quality of life, relieves pain, and enables a return to active living.
If all non-surgical methods have been tried and your pain can no longer be controlled, it may be time to consider surgical options. Some important signs we take into account when deciding on surgery include:
- Severe pain that wakes you at night and does not improve with rest
- Lack of response to non-surgical treatments and strong painkillers
- Walking distance reduced to below a few hundred meters, even difficulty moving inside the house
- Inability to perform basic daily activities such as putting on socks, tying shoes, or getting up from a chair without help
- Constant pain and restricted mobility causing withdrawal from social life and serious decline in quality of life
If one or more of these apply to you, unnecessarily delaying surgery can cause further muscle weakening, worsening of bone deformity, and deterioration of general health, making recovery more difficult after surgery. Therefore, making the surgical decision at the right time with a specialist is very important. Today, the gold standard surgical treatment for hip osteoarthritis is Total Hip Replacement surgery. In this procedure, the worn joint surfaces are replaced with modern and durable implants, creating a new joint that is painless and mobile.
What Should People with Hip Osteoarthritis Pay Attention to in Their Diet?
Healthy and balanced nutrition plays a critical role not only for overall health but also for joint health. In the case of hip osteoarthritis, diet has two main goals. The first is to help maintain an ideal weight to reduce the mechanical load on the joint. The second is to prefer foods that reduce inflammation in the body and support cartilage tissue. With some simple changes at your dining table, you can support your joints.
Some food groups that support joint health:
- Omega-3 fatty acids (fatty fish such as salmon, mackerel, sardines, walnuts, flaxseeds)
- Antioxidant-rich fruits (dark-colored fruits such as blueberries, strawberries, blackberries, cherries)
- Green leafy vegetables (spinach, kale, chard, broccoli)
- Olive oil (especially extra virgin olive oil)
- Spices (turmeric and ginger)
- Foods supporting bone and cartilage (bone broth, tripe soup)
- Adequate calcium and vitamin D (dairy products, green vegetables, sunlight)
Foods you should limit because they can increase inflammation in the body:
- Processed sugar (sugary drinks, packaged sweets, pastries)
- Foods containing trans fats (fried foods, margarine, processed baked goods)
- Processed meat products (salami, sausage, cured meats)
- Excessive salt intake
- Excessive alcohol consumption
Remember, no single food can work miracles. What matters is making balanced and varied eating habits a part of your lifestyle.
How Does Hip Osteoarthritis Affect Psychology and Daily Life?
Hip osteoarthritis is not just a problem of bones and cartilage. This condition can deeply affect a person’s entire life, mood, and social relationships. Living with constant, unpredictable pain is exhausting and frustrating in itself. Not being able to go for enjoyable walks, play comfortably with your grandchildren, or make travel plans with friends… All of these can eventually lead to feelings of inadequacy and helplessness.
Fear of movement (kinesiophobia) may develop. The person may think, “What if it hurts more if I move?” and start avoiding activity, leading to a more sedentary lifestyle. This inactivity both weakens the muscles and causes weight gain, which worsens osteoarthritis symptoms in a vicious cycle.
During this process, social isolation, loss of enjoyment of life, hopelessness, and even depression are common. If you are experiencing these feelings, you should know that this is completely normal and understandable. You are not the only one going through this. Paying attention to your mental health during treatment and seeking psychological support when necessary is an important part of recovery. True healing occurs when a pain-free body is combined with a peaceful mind.
Contact us for detailed information and an appointment!
Frequently Asked Questions
What is hip osteoarthritis and why does it occur?
Hip osteoarthritis is a joint disease that occurs when the cartilage tissue in the hip joint wears down and thins over time, leading to pain and restricted movement. The most common causes are aging, excessive weight, previous hip injuries, congenital hip dislocation, and certain rheumatic diseases.
What are the symptoms of hip osteoarthritis?
The most common symptom is pain felt in the groin, hip, or thigh area. Morning stiffness, pain that increases when climbing stairs or walking, movement restrictions, stiffness in the hip, and sometimes limping may be observed. In advanced stages, joint noises such as clicking and deformities may develop.
How is hip osteoarthritis diagnosed?
Diagnosis is made primarily by a doctor’s examination and evaluation of the patient’s complaints. X-rays, MRI, and sometimes blood tests are used to determine the severity of osteoarthritis and detect other joint problems.
What treatment methods are applied in hip osteoarthritis?
Treatment includes medication use, weight control, exercise, physical therapy, intra-articular injections, and pain management methods depending on the stage of the disease. In advanced cases, hip replacement surgery may be considered.
Is it possible to completely cure hip osteoarthritis?
Osteoarthritis is a progressive disease and cannot be completely cured. However, with proper treatment, pain can be reduced, and joint mobility can be preserved. Surgery can provide significant relief and improved mobility.
What should someone with hip osteoarthritis pay attention to in daily life?
Weight control, regular exercise, avoiding jumping and sudden movements, choosing proper footwear, and avoiding prolonged standing are important. In addition, stair use should be minimized, and support should be used when sitting and standing up.
Can hip osteoarthritis be seen in young people?
Yes, especially in cases of congenital hip dislocation, previous hip fractures, or joint injuries, osteoarthritis may develop at a young age. In younger patients, treatment planning is done more carefully.
Which exercises are good for hip osteoarthritis?
Swimming, water exercises, light walking, and hip-strengthening exercises performed under the guidance of a physiotherapist are recommended. High-impact activities involving jumping or sudden turns should be avoided.
When does surgical treatment come into question for hip osteoarthritis?
If pain persists despite medication and physical therapy, if daily life activities are severely restricted, and if joint mobility is significantly reduced, surgical treatment, especially hip replacement surgery, may be considered.
Does hip osteoarthritis cause permanent disability?
If not treated properly, osteoarthritis can cause severe joint damage and deformity over time, leading to permanent disability. Early diagnosis and correct treatment can significantly reduce this risk.