Prof. Dr. Murat Demirel, one of the best orthopedic doctors performing hip replacement surgery in Ankara, offers modern and permanent solutions to his patients with advanced hip osteoarthritis, cartilage wear, fractures, or severe damage to the joint surface. Hip replacement surgery is an advanced surgical method that aims to relieve pain, improve mobility, and increase quality of life by replacing damaged joint surfaces with artificial prostheses. Prof. Dr. Demirel provides patient-specific surgical plans in centers equipped with advanced medical technology and high hygiene standards among hospitals performing hip replacement surgeries in Ankara.
By conducting detailed evaluations before surgery, Prof. Dr. Demirel determines the most suitable type of prosthesis and surgical technique, and he also closely monitors his patients after surgery. With doctor’s recommendations after hip replacement surgery, he ensures that the recovery process is safe, fast, and long-lasting. In addition, he provides transparent and up-to-date information about hip replacement surgery costs in Ankara, helping his patients make informed decisions. You can also contact us immediately to schedule an appointment and regain the freedom of pain-free movement and improve your quality of life.
| Surgery Name | Hip Replacement Surgery (Total Hip Arthroplasty) |
| Application Area | Hip joint (acetabulum and femoral head) |
| Indications | Hip osteoarthritis, avascular necrosis, rheumatoid arthritis, post-fracture sequelae, hip dysplasia |
| Surgical Method | Open surgery; replacement of damaged joint surfaces with metal and polyethylene prostheses |
| Type of Anesthesia | Spinal, epidural, or general anesthesia |
| Operation Duration | Usually 1.5–2 hours |
| Hospital Stay | Average 3–5 days |
| Recovery Period | 6–12 weeks; full functional recovery 3–6 months |
| Complications | Infection, prosthesis loosening, dislocation, leg length discrepancy, nerve injury |
| Advantages | Elimination of hip pain, increased mobility, improved quality of life |
| Alternative Methods | Conservative treatments (medication, injection, physical therapy), osteotomy |
| Suitable Patient Profile | Individuals with advanced hip osteoarthritis, pain affecting daily life, and no response to other treatments |


Prof. Dr. Murat Demirel
Orthopedics and Traumatology Specialist
Orthopedics Specialist Prof. Dr. Murat Demirel was born in Ankara in 1974. He completed his primary education at Ankara Kavaklıdere Primary School and his secondary and high school education at Ankara Atatürk Anatolian High School. Dr. Demirel graduated from Ankara University Faculty of Medicine in 1998 and completed his residency in Orthopedics and Traumatology at Ankara Numune Training and Research Hospital, 1st Orthopedics and Traumatology Clinic, in 2004.
PhD
Ankara University Institute of Health Sciences
Specialization
Ankara Numune Training and Research Hospital, 1st Orthopedics Clinic
Medical School
Ankara University Faculty of Medicine
Yazı İçeriği
What is Hip Replacement Surgery and Why is it Necessary?
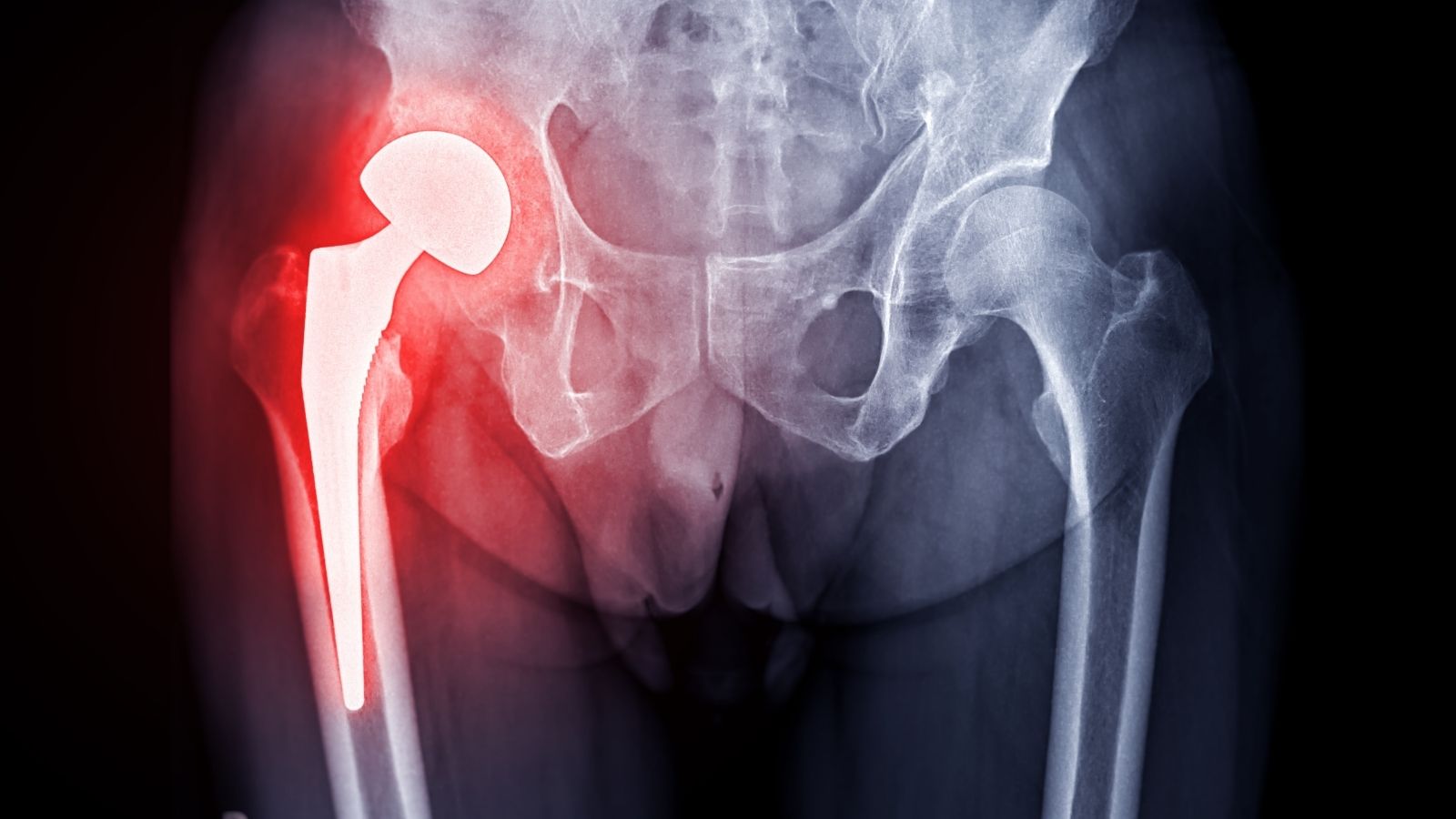
In the simplest terms, hip replacement surgery is the surgical removal of your hip joint, which has lost its function and causes severe pain for various reasons, and replacing it with an artificial joint (prosthesis) that mimics movement and function. Medically referred to as “total hip arthroplasty,” in this procedure, the orthopedic and traumatology surgeon meticulously cleans the damaged cartilage and bone tissues in the two main parts of your hip joint — the socket in your pelvis (acetabulum) and the head of your thigh bone (femoral head). Modern implants made of biocompatible metal alloys, special ceramics, and highly durable plastic called polyethylene are then placed. This new artificial joint is designed to precisely mimic the hip’s natural “ball and socket” mechanism. Thus, our goal is to eliminate pain while preserving the naturalness of your movements at the highest level.
So, what are the reasons that lead a person to hip replacement surgery? The main conditions that make this surgery necessary are as follows:
Osteoarthritis (Degenerative Joint Disease): The most common reason for hip replacement surgery. Over the years, the protective cartilage in the joint wears down and thins, causing bones to rub against each other. This results in severe pain, difficulty in movement, and joint stiffness. While it usually occurs with age, genetic predisposition or previous joint injuries can accelerate this process.
Rheumatoid Arthritis and Other Inflammatory Arthritides: These are autoimmune conditions in which the immune system mistakenly attacks its own joint tissues. The synovial membrane covering the joint becomes inflamed, which over time destroys cartilage and underlying bone, causing severe pain and deformities.
Avascular Necrosis (Osteonecrosis): The collapse of bone tissue due to disruption of blood flow to the femoral head. This condition may develop after hip fractures, dislocations, or long-term use of certain medications such as corticosteroids, and it can lead to hip replacement even in young patients.
Post-Traumatic Arthritis: Arthritis that develops years after a major hip injury such as a fall or traffic accident, resulting from fractures or damage sustained earlier.
Childhood Hip Disorders: Conditions such as congenital hip dislocation or Perthes disease during childhood may affect hip development and cause early degeneration, leading to a need for prosthesis later in life.
Developmental Hip Dysplasia: A congenital structural abnormality of the hip joint where the socket does not adequately cover the femoral head. This abnormal load bearing leads to early arthritis. It is particularly common in young women and is a frequent reason for hip replacement.
The decision for surgery is usually made when other treatment methods are exhausted. If you experience one or more of the following, hip replacement surgery may be the right option for you. Here are some important signs indicating that surgery is necessary:
- Hip pain that continues even while resting during the day
- Pain that wakes you up at night or prevents you from falling asleep
- Significant difficulty with movements such as climbing stairs or getting in and out of a car
- Severe pain when bending to put on socks or shoes
- Walking distance gradually decreasing due to pain, even when using a walker or cane
- Pain medications no longer working or requiring high doses
- Having to give up social activities and hobbies you enjoy due to pain
These symptoms indicate that your hip problem is no longer just a joint issue but is threatening your overall health, mood, and social independence. The goal of hip replacement surgery is not only to eliminate pain but also to give you your life back.
Who is a Good Candidate for Hip Replacement Surgery?
Determining whether you are the “right time” or “right candidate” for hip replacement surgery is a decision made jointly by you, your family, and your orthopedic surgeon. There is no absolute age or weight limit. The main criterion is how much your hip pain and functional loss affect your quality of life and whether non-surgical treatments are no longer helpful. While this surgery was once considered mainly for older patients, thanks to advancing technology, younger and active patients now also greatly benefit from it.
A comprehensive evaluation is performed to determine a patient’s suitability for hip replacement surgery. This process generally includes the following steps:
Detailed Medical History: Your doctor carefully reviews your general health status, past illnesses, medications you regularly use, and the history of your hip pain (when it started, how it progressed, what activities worsen it, etc.).
Physical Examination: Your surgeon examines the range of motion of your hip, your muscle strength, your gait (whether you limp), your leg lengths, and pinpoints where the pain occurs.
Imaging Methods: Standard X-rays are usually sufficient to assess the degree of joint damage, cartilage loss, and bone deformities. In certain cases, especially avascular necrosis or when soft tissues around the joint need more detailed evaluation, additional imaging such as MRI or CT may be requested.
Based on this evaluation, patients who meet the following criteria are generally considered good candidates for hip replacement surgery:
- Severe hip pain unresponsive to non-surgical treatments (medications, physical therapy, joint injections).
- Clear evidence of joint damage on X-rays.
- Serious limitations in daily activities (walking, climbing stairs, dressing).
- No uncontrolled major health problem (such as active infection, severe heart or lung disease) that would increase surgical risk.
Every patient is different, and the decision for surgery is made individually. The goal of the surgery is to restore the right to move without pain and enjoy life for individuals of all ages.
Contact us for detailed information and an appointment!
What Surgical Approaches Are Used in Hip Replacement Surgery?
During hip replacement surgery, the surgeon can use several different routes (surgical approaches) to access the damaged joint. All these approaches serve the same basic purpose: to remove the damaged joint and place the prosthesis. However, the path they take to reach the joint, meaning the muscles and tissues they cut or separate, varies. Your surgeon will choose the most appropriate approach based on your anatomy, weight, bone quality, and their own experience. Remember, the best approach is the one your surgeon is most experienced with and believes will achieve the best outcome for you. The main surgical approaches are as follows:
Posterior Approach: The most commonly used method worldwide, also known as the “traditional” approach. The incision is made on the back-side of the hip, over the buttock. This approach allows the surgeon a wide field of vision and easy placement of the prosthesis. In this method, some of the small muscles that enable external rotation of the hip may need to be cut and then reattached at the end of the surgery. After surgery, it is important to avoid certain movements (such as crossing legs) until these muscles heal.
Anterior Approach: A more “muscle-sparing” technique that has gained popularity in recent years. The incision is made at the front of the hip, and the surgeon reaches the joint through natural spaces between muscles instead of cutting them. Its main advantage is less pain in the early postoperative period, faster recovery, and potentially lower dislocation risk because the main muscle groups are preserved. However, not every patient is suitable for this approach, and it requires special experience from the surgeon as it can be technically more challenging.
Lateral Approach: The incision is made directly on the side of the hip. This approach also provides good visualization and allows stable placement of the prosthesis. In this method, some of the muscles responsible for lifting the leg to the side (abductor muscles) may need to be partially separated. This can cause temporary limping after surgery in some patients, but with a good physical therapy program, it usually improves.
What Materials and Types of Prostheses Are Used in Hip Replacement Surgery?
A hip prosthesis is much more than just a piece of metal; it is a biomechanical marvel made up of several main components. The materials used and the way it attaches to the bone directly affect the lifespan and performance of your prosthesis. Your surgeon will choose the most suitable prosthesis combination for you, considering your age, activity level, bone quality, and overall health condition.
Main Components of the Prosthesis
A hip prosthesis basically consists of four parts.
Acetabular Cup (Socket): A metal cup that replaces the damaged socket in the pelvis. It is usually made of a biocompatible metal such as titanium.
Liner (Insert): A smooth surface placed inside the metal cup, where the ball moves. This part is one of the most important components that determine the wear resistance and longevity of the prosthesis.
Femoral Stem: A long metal stem inserted into the thigh bone (femur). It is also made of metals such as titanium.
Femoral Head (Ball): The ball-shaped component attached to the stem that moves inside the liner, providing joint movement.
Fixation Methods
How the prosthesis attaches to the bone is also crucial. There are two main methods.
Cementless Fixation: In this method, the surface of the prosthesis has a rough, porous coating that encourages bone growth into it. The prosthesis is tightly fitted into the bone canal (“press-fit”). Over time, the bone naturally integrates with the porous surface, fixing the prosthesis very securely. It is generally preferred in younger, more active patients with good bone quality.
Cemented Fixation: In this method, a special filler material called “bone cement” (polymethylmethacrylate) is placed between the prosthesis and the bone to glue the prosthesis in place. Cement provides immediate fixation. Therefore, it is often preferred in elderly patients with weaker bone quality (e.g., osteoporosis), as it allows them to put weight on the leg immediately after surgery.
Hybrid Fixation: Sometimes a combination of both methods is used. For example, the cup may be placed without cement, while the stem is cemented.
Articulation Surfaces (Bearing Combinations)
One of the most critical factors determining the longevity of the prosthesis is the materials used in the friction surfaces between the ball and the liner. Here are the main combinations used today:
Metal-Polyethylene: A metal ball moves inside a polyethylene (special hard plastic) liner. It has been used for many years, is reliable, and cost-effective. Thanks to modern “cross-linked” polyethylene, wear rates have been significantly reduced.
Ceramic-Polyethylene: A ceramic ball moves inside a polyethylene liner. Since ceramic is smoother and more scratch-resistant than metal, it causes less wear on the polyethylene insert, thereby extending the prosthesis lifespan. It is also a good alternative for patients with metal allergies.
Ceramic-Ceramic: Both the ball and the liner are made of ceramic. It has the lowest wear rates known. Therefore, it is an ideal option for very young, active patients with a long life expectancy. The risk of ceramic fracture, which was a concern in the past, has been significantly reduced with modern third- and fourth-generation ceramics.
Ceramic-Metal: This combination can also be used but is less common.
Metal-Metal: Although used in the past, it has been almost completely abandoned today because the metal ions released from friction between metal surfaces can accumulate in the body and cause various problems (metallosis).
How Does the Preparation Process Before Hip Replacement Surgery Progress?
The success of hip replacement surgery depends not only on the few hours spent in the operating room but also on the proper preparations made in the weeks before surgery. This process aims to prepare both your body and your home for the recovery period after surgery.
Medical Preparations
- A series of medical evaluations will be required a few weeks before your surgery.
- General Health Check: Before surgery, you will be examined by the anesthesiologist and usually an internal medicine or cardiology specialist. They will assess whether you have any condition that might prevent surgery.
- Medication Adjustment: It is vital to inform your doctor about all the medications you use (prescription, over-the-counter, herbal supplements). Especially blood thinners (Aspirin, Coumadin, Plavix, etc.) may need to be discontinued or replaced with another medication a certain time before surgery.
- Blood and Other Tests: Standard preoperative tests include blood count, clotting tests, kidney and liver function tests, urinalysis, chest X-ray, and heart electrocardiogram (ECG).
- Dental Check: An infection focus in the body can spread through the blood to your new prosthesis. Therefore, if you have problems such as cavities or gum disease, you may be asked to have them treated by a dentist before surgery.
- Infection Screening: In some cases, additional screening may be performed to check for hidden infection sources in the body.
Lifestyle Changes
- There are some important steps you can take to improve surgical outcomes and reduce risks.
- Quit Smoking: Smoking slows blood circulation, delays wound healing, and increases infection risk. It is strongly recommended to quit smoking at least 4–6 weeks before surgery.
- Weight Control: Excess weight can cause technical difficulties during surgery and increase the load on your new prosthesis, shortening its lifespan. Your doctor may recommend losing weight before surgery.
- Nutrition: A balanced diet rich in protein and vitamins before and after surgery will strengthen your body’s healing ability.
Home Preparation
- Making certain adjustments at home will make your recovery period more comfortable and safer after returning from the hospital.
- Remove small rugs, carpets, and cables that may cause you to trip and fall in walking areas.
- Place frequently used items (phone, remote control, book, water) within easy reach, such as on a table next to your bed or chair.
- Use non-slip mats in the bathroom, consider adding a shower stool and grab bars on the walls. A raised toilet seat will also make sitting and standing easier.
- Plan support with a family member or friend who can help you during the first few weeks after surgery.
- Prepare easy-to-heat, portioned meals in advance and store them in the freezer.
How Does the Recovery Process Work After Hip Replacement Surgery?
Recovery after hip replacement surgery is like a marathon, not a sprint. Everyone’s healing pace is different, and it is very important to be patient, listen to your body, and strictly follow the instructions of your doctor and physiotherapist during this process.
The First Days in the Hospital (Usually 1–3 Days)
- After surgery, you will be monitored in the recovery room for a while before being taken to your room.
- On the day of surgery or the following day, your physiotherapist will visit you to perform the first exercises and help you stand up.
- This early mobilization is critical to prevent serious complications such as blood clots.
- Initially, you will walk with the help of a walker.
- Your pain will be managed with intravenous or oral medications.
- To prevent fluid buildup in your lungs, you will be asked to use a special breathing exercise device and practice frequent deep breathing and coughing.
The First Weeks at Home (2–6 Weeks)
- This period is when recovery is fastest but also when you must be most careful.
- You should care for your surgical wound as instructed. Keeping the wound clean and dry is important.
- Take the prescribed medications regularly for pain control.
- Elevating your leg above heart level while resting and applying ice regularly will help reduce swelling and pain.
- Perform the home exercise program shown by your physiotherapist several times a day without skipping. These exercises will strengthen your muscles and restore your joint mobility.
- Continue using a walker or crutches. Your doctor or physiotherapist will tell you when you can switch to a cane or walk without assistance.
- Your first postoperative check-up usually occurs in the 2nd or 3rd week. At this visit, your stitches may be removed, and X-rays will be taken to ensure everything is on track.
Later Stage (6 Weeks – 3 Months)
- During this period, your strength and mobility will significantly improve, and you will gradually return to normal life.
- Most patients can start driving again during this time (but you must get your doctor’s approval).
- You can start low-impact exercises such as walking. Increase your walking distance gradually.
- The need for assistive devices will decrease or disappear completely.
- You can resume more active household tasks and social activities.
Full Recovery (3 Months and Beyond)
Full recovery, meaning reaching your maximum potential with your new hip, may take 6 months to 1 year. Regaining muscle strength and endurance takes time. It is important to continue regular exercise during this period. With your doctor’s approval, you may begin low-impact sports such as swimming, cycling, golf, or dancing. However, it is generally recommended to avoid high-impact activities such as running or jumping to prolong the life of your prosthesis.
What Are the Possible Risks and Complications of Hip Replacement Surgery?
Although hip replacement surgery is one of the safest and most successful procedures in orthopedics, like any surgical operation, it carries certain risks and potential complications. These risks are quite low, and both the surgical team and you will take all necessary precautions to minimize them. Knowing these risks is important for making an informed decision and for recognizing possible problems early in the postoperative period.
Infection: Infection may develop at the surgical site or around the prosthesis. With sterile operating room conditions, antibiotics given before and after surgery, and your adherence to hygiene rules, this risk is reduced to below 1%. If a deep infection develops, additional surgeries may be required, and in some cases, the prosthesis may need to be removed.
Blood Clot (Deep Vein Thrombosis and Pulmonary Embolism): After surgery, blood clots may form in the leg veins. If such a clot breaks loose and travels to the lungs (pulmonary embolism), it can be life-threatening. To prevent this, blood-thinning medications, compression stockings, and, most importantly, early mobilization are used after surgery.
Prosthesis Dislocation: This is when the artificial joint’s ball component slips out of its socket. It may occur especially in the first few months after surgery due to sudden or wrong movements. Therefore, it is very important to follow the movement restrictions taught to you.
Leg Length Difference: Your surgeon will take great care to equalize your leg lengths during surgery. However, sometimes the operated leg may end up slightly longer or shorter. This difference is usually minimal and may not be noticeable. If necessary, it can be corrected with a small shoe lift.
Loosening and Wear of the Prosthesis: Over the years, prosthetic components may wear down or lose their attachment to the bone, causing loosening. Modern prostheses typically last over 20–25 years, but excess weight and high-impact activities can shorten this lifespan. Loosening causes pain and may require revision (second) surgery.
Periprosthetic Fractures: Fractures in the bone around the prosthesis may occur during or after surgery, especially due to a fall. These often require additional surgical intervention.
Nerve and Blood Vessel Injury: Very rarely, large nerves or blood vessels near the surgical site may be injured.
Frequently Asked Questions
Who is hip replacement surgery recommended for?
Hip replacement surgery is generally recommended for older patients who experience severe pain and movement limitations due to advanced hip osteoarthritis, fractures, congenital hip dislocation, or certain rheumatic diseases, and who no longer benefit from other treatment methods.
What is the recovery process like after hip replacement surgery?
During recovery, patients are usually encouraged to stand up on the first day after surgery. The average hospital stay is 3–5 days. Most of the healing occurs within the first 6–8 weeks. With physiotherapy and regular exercise, full functional recovery may take 3–6 months.
Is hip replacement surgery a risky operation?
As with any surgical procedure, hip replacement surgery carries certain risks. Complications such as infection, blood vessel or nerve injury, blood clots, prosthesis loosening, or dislocation can occur, though rarely. With an experienced medical team and proper conditions, the success rate is very high.
What should be considered after hip replacement surgery?
In the first few weeks after surgery, sudden movements, sitting on low chairs, and crossing the legs should be avoided. The doctor’s recommended exercises and physiotherapy should be performed regularly, and wound care and medications should not be neglected.
How long does a hip prosthesis last?
Modern hip prostheses generally last around 15–20 years. Their longevity depends on the patient’s age, weight, activity level, and attention to postoperative care.
Can people with hip prostheses do sports?
After hip replacement, low-impact activities such as swimming, walking, and light cycling are recommended. Contact sports or activities requiring sudden movements should be avoided. Patients should always consult their doctor before starting any exercise.
Is there pain after surgery?
Mild to moderate pain may occur in the first days after surgery. This pain is usually controlled quickly and is expected to gradually decrease and disappear. In cases of severe or persistent pain, the doctor should be consulted.
When can patients return to daily life after hip replacement surgery?
Most patients can return home within the first week after surgery. Simple daily tasks can usually be resumed within 3–6 weeks. Driving is generally possible after 6–8 weeks, while a full return to social life takes about 3–6 months.
Is hip replacement surgery performed in state hospitals?
In Turkey, hip replacement surgery is performed in both state and private hospitals. In state hospitals, a significant portion of the cost is covered by SGK (Social Security Institution). In private hospitals, fees may differ.
Can loosening or dislocation of the prosthesis occur after hip replacement surgery?
Although rare, prosthesis loosening or dislocation may occur over time. This usually happens due to the natural lifespan of the prosthesis or because of excessive strain or improper movements after surgery. In such cases, additional surgery may be required.